JAMA Oncology:MUC16突变与更高的肿瘤突变量和更好的胃癌生存相关
2018-08-19 肿瘤资讯编辑部 肿瘤资讯
胃癌是一类基因异质性较大的疾病,肿瘤突变量(TMLs)存在显著差异。MUC16是胃癌中最常见的突变基因,但其与TML和患者预后的关系尚未明确。来自天津肿瘤医院的研究团队分别在TCGA胃癌队列和亚洲胃癌队列中独立验证了MUC16突变与胃癌突变量和患者生存的关系,并于近期发布在JAMA Oncology杂志上。
胃癌是一类基因异质性较大的疾病,肿瘤突变量(TMLs)存在显著差异。MUC16是胃癌中最常见的突变基因,但其与TML和患者预后的关系尚未明确。来自天津肿瘤医院的研究团队分别在TCGA胃癌队列和亚洲胃癌队列中独立验证了MUC16突变与胃癌突变量和患者生存的关系,并于近期发布在JAMA Oncology杂志上。
背景
胃腺癌是全球癌症病死率最高的肿瘤之一。尽管在HP根除和早期筛查上取得进展,但全球胃癌的5年生存率仅为29.6%。胃癌是一类基因异质性较大的疾病,肿瘤突变量(TMLs)存在显著差异。近期的研究显示,MSI-H或POLE突变的胃癌样本表现为DNA错配修复缺陷(MMR)和高的TMLs。在TCGA关于胃癌的分子亚型分类中,肿瘤突变量是重要的决定因素。在TCGA胃癌样本中,划分了4个不同的分子亚型,每个分子亚型的患者都有不同的基因特征。既往研究发现,胃癌的克隆复杂性和驱动突变模式与生存相关。近期研究显示,MMR缺陷的肿瘤,无论其组织学来源,均对免疫治疗敏感。MUC16是胃癌中最常见的突变基因,但其与TML和患者预后的关系尚未明确。本研究探索了MUC16突变与TML的关系,以及其是否影响胃癌患者的预后。
方法
研究从TCGA数据库中获取了437例胃癌患者的体细胞突变和基因表达数据;亚洲队列患者的临床和特细胞突变数据从既往的研究中获取。亚洲队列中包含256例胃癌患者,其中78例来自中国北方、100例来自香港、49例来自南韩、30例来自韩国。亚洲队列的基因表达数据未可及。肿瘤突变量定义为log2(每百兆碱基突变率)。
结果
TCGA队列
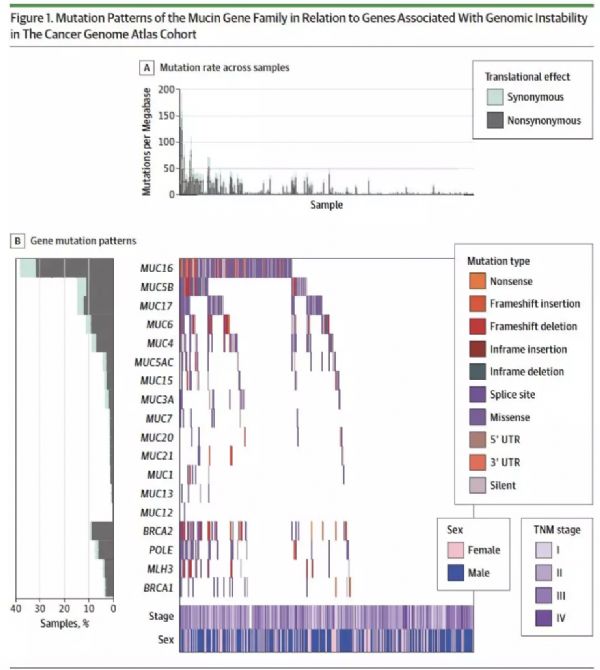
在437例胃癌患者中,280例(64.1%)为男性,中位年龄为67.6岁。TCGA队列中,最常见的突变基因之一为MUC16,突变率为38.4%(168/437)。合并MUC16突变的患者相比于无MUC16突变的患者,TMLs更高,见图1A。在MUC16突变的患者中,73例患者同时合并与维持基因完整性、DNA复制和MMR相关的基因突变,如BRCA1/2、POLE和MLH3,见图1B。MUC16和其家族成员之间的突变相关性总结见图1B。
图1. TCGA队列中,Mucin基因家族突变模式与基因不稳定相关基因突变的关系
MUC16突变与TML的关系
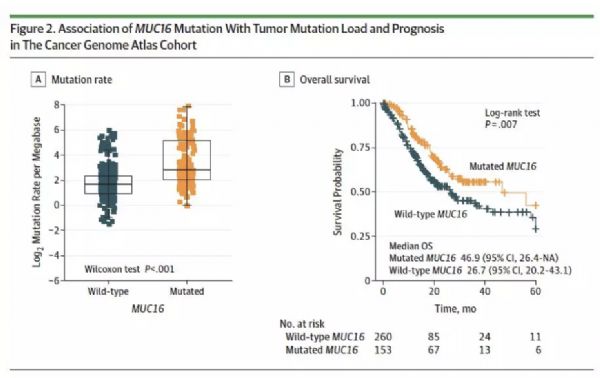
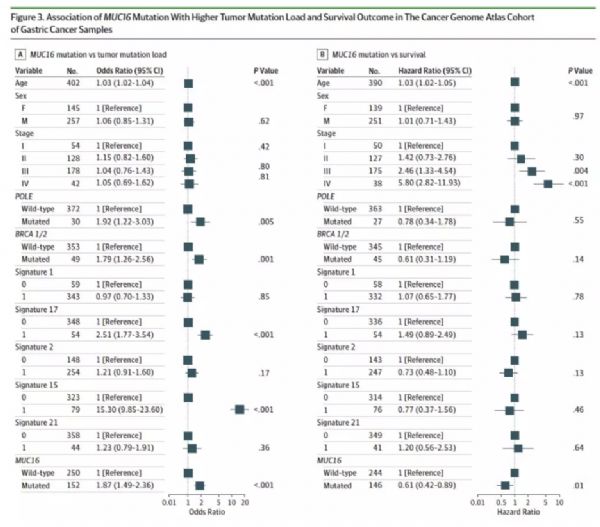
MUC16突变的胃癌样本具有更高的突变率,见图2A。治疗突变量主要与基因不稳定性相关,其在胃癌中很常见。在这些样本中,研究者发现了6个突变特征,包括与基因不稳定相关基因。在分析MUC16突变和TML关系时,研究者采用多因素模型,排除了潜在的混杂因素。在多因素分析中,MUC16突变和TML显著显著相关(OR 1.87,P<0.001),图3A。
TCGA队列患者的生存
在TCGA队列中,MUC16突变与更好的生存显著相关(mOS 46.9 vs 26.7,P=0.007)。在校正了年龄、性别、TNM分期、BRCA1/2和POLE突变以及dMMR后,仍存在显著差异,HR 0.61(95%CI:0.42-0.89),P=0.01,图3B。
图2. TCGA队列中,MUC16突变和TML及预后的关系
图3. TCGA队列中,MUC16突变与更高的TML和更好的预后相关
亚洲队列中,独立验证MUC16突变
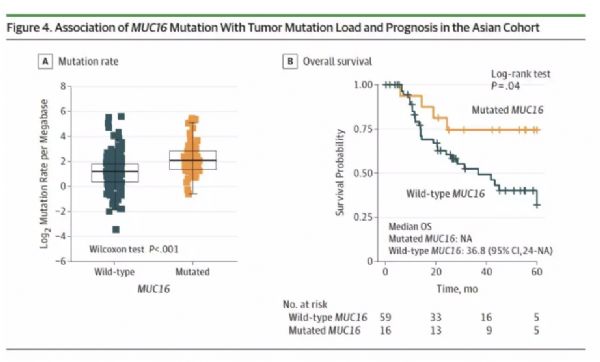
亚洲队列中纳入256例患者,其中141例为男性,中位年龄为63岁。MUC16突变在亚洲人群中突变率为22.3%。在MUC16突变的胃癌患者中,观察到显著更高的突变数(134 vs 74,P<0.001)。与TCGA队列相似,MUC16突变的胃癌患者,相比于无突变的患者,有显著更高的TML(2.1 vs 1.2,P<0.001),见图4A。MUC16突变与更高TML的相关性在调整年龄、性别、TNM分期、突变特征和BCA1/2突变,POLE突变的多因素模型中,仍存在显著统计学意义(OR 1.69;95%CI:1.25-2.29;P<0.001),见图5A。在生存分析中,MUC16突变与更好的预后显著相关,见图4B,mOS分别为尚未达到 vs 36.8个月,P=0.04;在调整了年龄、性别、TNM分期和突变特征后,差异仍有显著统计学意义(HR 0.26;95%CI:0.07-1.02;P=0.05),见图5B。
图4. 亚洲队列中,MUC16突变和TML及预后的关系
图5. 亚洲队列中,MUC16突变与TML和生存的关系
结论和讨论
在TCGA和亚洲队列这2个独立的基因数据库中,研究发现MUC16突变和更高的TML相关,也与胃癌患者更好的预后相关。这一结果有助于判断胃癌患者的预后,并指导临床治疗。
原始出处:
Xiangchun Li, Boris Pasche, Wei Zhang, et al. Association of MUC16 Mutation With Tumor Mutation Load and Outcomes in Patients With Gastric Cancer. JAMA Oncology. Aug 2018.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Oncology#
47
#Oncol#
37
#肿瘤突变#
38
学习了,谢谢作者分享!
80
学习了谢谢
82