Frontiers in Cellular and Infection Microbiology:肠道菌群在子宫内膜异位症的早期诊断上优于宫颈粘液菌群
2021-12-20 “生物世界”公众号 “生物世界”公众号
子宫内膜异位症(EM)是一种雌激素依赖的女性常见病,子宫内膜腺体和间质在子宫腔以外的部位种植生长,盆腹腔是其最常见的发病部位。EM可致痛经、不孕、盆腔粘连,甚至恶变。由于病因不明。
子宫内膜异位症(EM)是一种雌激素依赖的女性常见病,子宫内膜腺体和间质在子宫腔以外的部位种植生长,盆腹腔是其最常见的发病部位。EM可致痛经、不孕、盆腔粘连,甚至恶变。由于病因不明,目前缺乏治“本”疗法,除根治性手术外,普通药物或常规手术治疗后的复发率甚至超过50%。
由于缺乏特异性的症状以及血清标记物,EM难以实现早期无创诊断。异常的炎性反应参与了EM的发病,肠道微生物群与多种炎症性疾病的发生相关,既往研究亦表明肠道、生殖道菌群与EM之间存在关联。目前尚未有研究利用配对样本阐明肠道菌群、生殖道菌群及EM病发部位盆腹腔菌群的相关性,且基于不同部位的菌群建立EM的早期预测模型的准确性仍存在较大差异,这也是EM研究领域的一个热点。
12月7日,南方医科大学珠江医院妇产医学中心马颖教授团队联合广东省微生物研究所肠道微生态与健康团队PI谢黎炜研究员,在 Frontiers in Cellular and Infection Microbiology 期刊上发表了题为:Gut Microbiota Exceeds Cervical Microbiota for Early Diagnosis of Endometriosis 的观察性研究报告。
该研究首次报道了肠道菌群在子宫内膜异位症的早期诊断上优于宫颈粘液菌群,该研究通过采集EM患者及对照组内受试者粪便、宫颈粘液及腹腔冲洗液的配对样本进行菌群的分析,该研究的发现为后续EM与菌群相关性研究提供了全新的策略和方向。
子宫内膜异位症是一种慢性炎症性妇科疾病,生育期女性中的患病率可高达10%,影响了全球范围内上亿女性。EM是指子宫内膜腺体和间质种植在子宫腔以外的部位,其中盆腹腔为常见的病变部位。EM主要表现为盆腔疼痛,严重者影响生活质量,而目前,确诊盆腔内异症的金标准为腹腔镜检查加上病理检查。截至今日,对此病发病的机制有多种说法,而被普遍认可的是1927年Sampson提出的子宫内膜种植学说,由于子宫腔与盆腔之间通过输卵管连接,当经血逆流时原本位于子宫腔内的细胞可流经输卵管到达盆腔并种植于盆腔继而导致EM的发生。但是80%的生育期女性都有可能经历经血逆流,而EM在生育期女性的发病率不超过10%,这提示我们EM患者的盆腹腔微环境可能有所不同。
在传统观念中,上生殖道及腹腔为无菌的环境。随着科技的进步及高通量测序技术的应用,这一观念受到了前所未有的挑战。有研究表明,生殖道、腹腔及人体内多个部位均非绝对无菌的环境。而腹腔中的菌群有3个可能的来源:淋巴系统、循环系统及生殖道逆行传播。在过去几十年里,我们已经对微生物调控人体健康的重要性达成共识,菌群紊乱可能会干扰宿主的免疫调控系统并且导致一些炎症性疾病的发生。随着日新月异的科学技术应用于检测人类基因组,一系列分析工具也应运而生,专注于评估生物指标并挖掘疾病的生物标记物。鉴于此,寻找到能够早期无创诊断EM的目标标记物将会具有重大的意义。
既往已有大量研究报导肠道菌群参与调控机体免疫系统并参与炎症性疾病的发生发展,肠道菌群与EM的相关性也偶有报导。宫颈粘液为连通富含乳杆菌的阴道及相对无菌的子宫之间的宫颈管内的粘液栓,在生理结构上,宫颈粘液可堵塞宫颈管形成物理屏障阻止阴道微生物上行感染从而达到保护宿主的目的。可见,肠道菌群及宫颈粘液菌群作为无创可获取的生物样本,在EM的研究上具有重要意义。但是尚无研究尝试探索粪便、宫颈粘液及腹腔冲洗液样本之间的相关性,所以本研究基于多类型配对样本研究了EM患者肠道菌群、宫颈粘液菌群与腹腔菌群的相关性,并分别利用不同类型的样本建立了EM早期预测模型。
本研究纳入了21名符合EM诊断标准与20名对照组的女性受试者,入组前3个月未使用抗生素或药物。在入组时,均采集静脉血、粪便样本和宫颈粘液样本,并于腹腔镜手术中收集受试者的腹腔冲洗液。血液样本用于血液生化指标检测(结果无显着差异),粪便样本、宫颈粘液样本及腹腔冲洗液样本用于进行16S rDNA扩增子测序,通过16S rDNA扩增子测序,研究共获得122个配对样本并进行了一系列数据分析与挖掘(图1)。

图1 研究概况
首先,在进行数据分析前我们对于相对丰度低于1‰和亚组内占比小于10%的菌群进行了过滤,随后基于降噪后的数据我们对患有EM的受试者与对照组测序数据进行了分析。通过分别比较EM组与对照组内不同类型样本的菌群结构及多样性,我们发现在菌种水平上三个部位样本的菌群结构存在显着差异,且该三种样本共同拥有的菌种有19个(图2)。
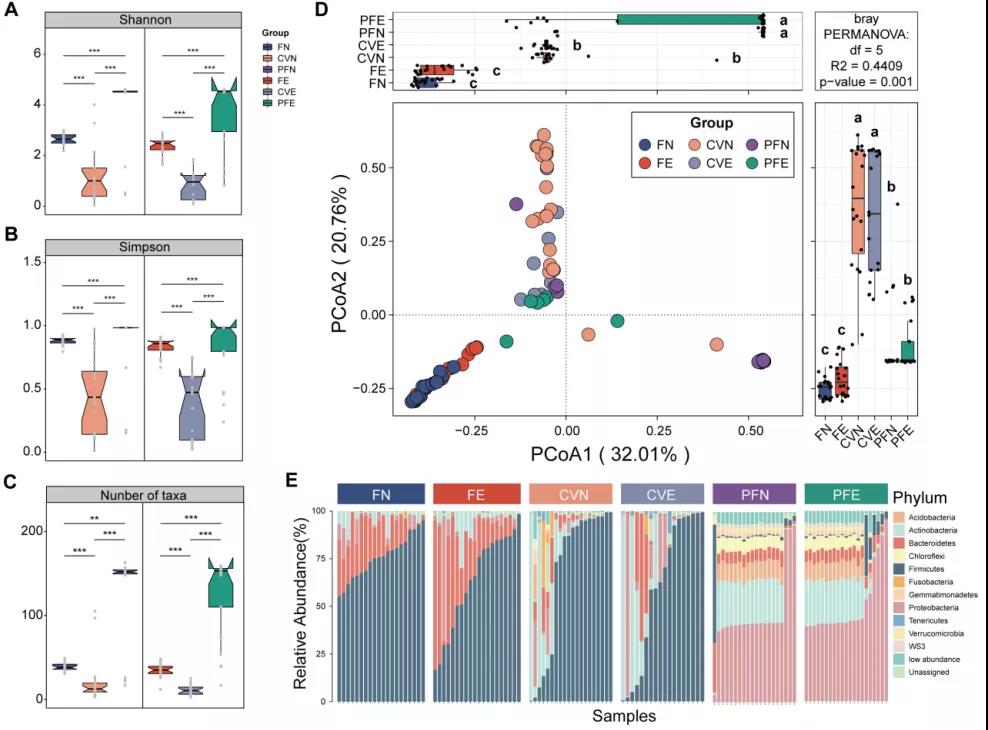

图2 不同类型样本菌群的结构
进一步分析在不同疾病状态下各部位的菌群多样性发现,EM组与对照组的肠道菌群在多样性上存在显着差异(图3A-D),而宫颈粘液菌群在组间并无显着差异(图3E-G),至于EM的病变部位盆腹腔环境的菌群丰富度无显着差异但在结构上可见差异(图3H-K)。既往研究中提示,肠道中Roseburia属(Clostridiales目,Clostridia科)能够产生丁酸,肠道中丁酸的减少会导致肠道上皮完整性受损继而通透性增大。在本研究中,Clostridiales Clostridia spp., Clostridiales Lachnospiraceae spp., 和Lachnospiraceae Ruminococcus sp.在EM组的肠道菌群中显着降低,参与机体代谢的肠道菌群的改变或许与机体的生理功能相关联,但尚无研究阐明这些差异菌与EM的相互关系。而在既往研究中表明可能在机体中产生负面影响的有害菌Eggerthella lenta在EM组肠道中显着富集。
以上结果提示我们有益菌的减少可能是促使有害菌的富集的触发因素,并且参与诱导机体的炎症反应。总的来说,EM组与对照组的肠道菌群结构与多样性存在显着差异,EM组肠道中的有害菌丰度增高而有益菌的丰度降低。
在分析EM组与对照组的腹腔冲洗液样本时发现,EM组样本中革兰阴性菌丰度显着增加,包括具有分泌脂多糖潜能的Pseudomonadaceae Pseudomonas sp. 和 Prevotellaceae Prevotella sp.。而细菌脂多糖 (LPS) 已被证实能够识别诱导巨噬细胞产生和分泌较高水平的促炎细胞因子TNF-α、IL-1α、IL-1β、IL-6、IL-12、IL-23和环氧合酶-2 (COX-2),而促炎细胞因子可促使子宫内膜异位基质细胞的增殖。此部分研究结果提示肠道菌群与腹腔冲洗液菌群结构可能对EM的发生发展产生影响。
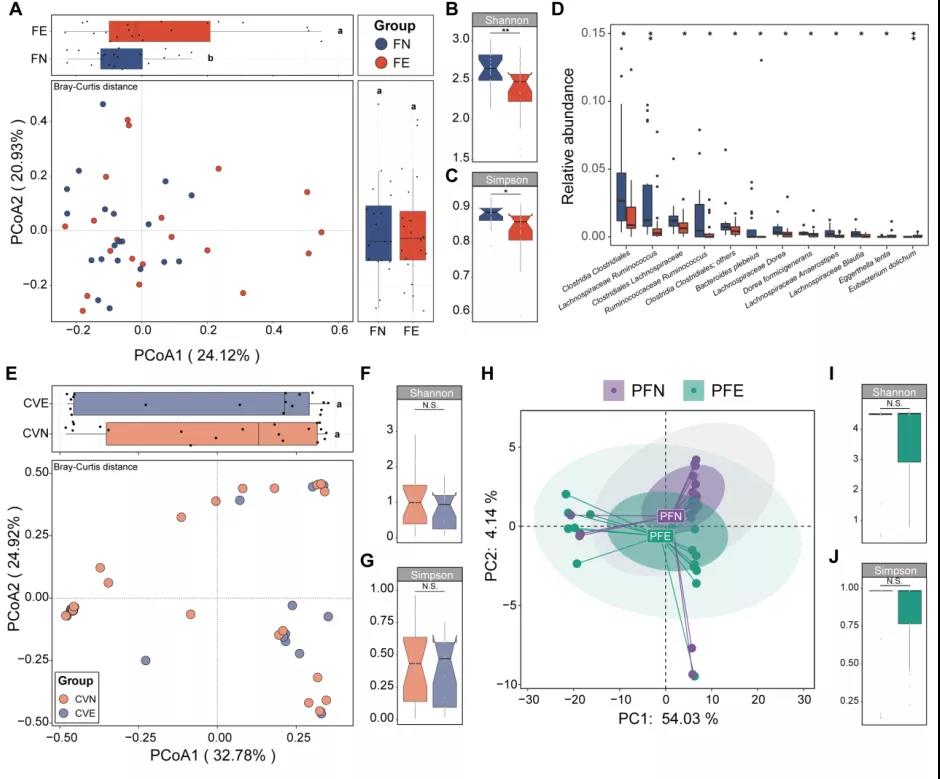
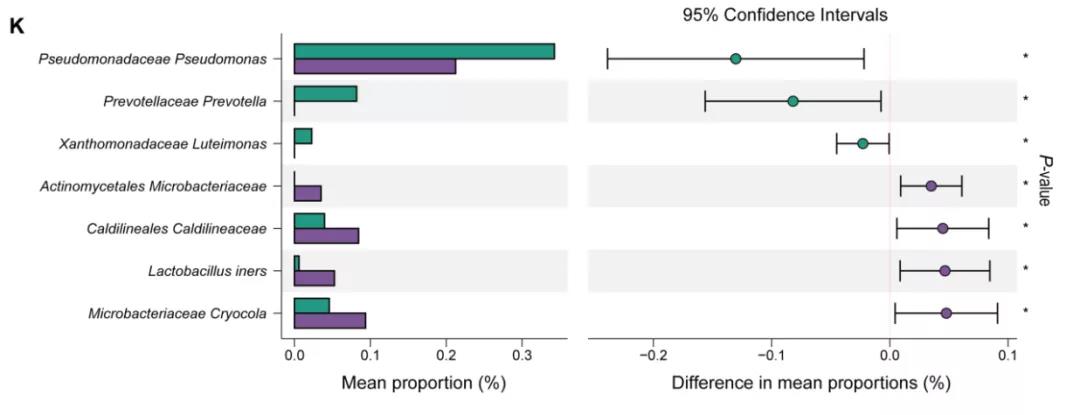
图3 不同类型样本菌群的差异
随后,我们应用了随机森林五交叉验证分别对三个部位的菌种进行筛选分析(图4A-B),综合十次模型分析结果取最优结果得出在肠道菌群中的关建菌Lachnospiraceae Ruminococcuss sp.(图4C)及腹腔冲洗液中的关建菌Pseudomonadaceae Pseudomonas sp.(图4D)。在既往研究中曾报道Ruminococcus faecis 与短链脂肪酸的产生成正相关,尤其是丁酸盐的合成。丁酸盐在大量文献中被证实与结肠癌和炎症相关,而EM的特征包括免疫失调和局部炎症,据此我们提出猜想,Lachnospiraceae Ruminococcuss sp.的减少可能通过代谢途径与EM存在相互关系。EM作为一种雌激素依赖性疾病,其特征是雌激素通过雌激素受体介导信号通路调控异位子宫内膜粘附、侵袭和血管生成的机制。已有研究提示,EM患者异位病灶中的局部雌激素浓度明显升高,但是血清中的雌激素水平可无明显改变。而铜绿假单胞菌(Pseudomonas aeruginosa)中含有的芳基硫酸酯酶A(arylsulphatase A)能够参与雌激素的生成。在我们的研究结果及前人研究结果均显示,EM组的腹腔冲洗液相比于对照组样本含有更高丰度的假单胞菌属,我们猜测假单胞菌的增加有可能通过参与雌激素代谢继而调控异位的子宫内膜组织。
在进一步的种级别水平的共发生网络分析中,我们进一步探索了机体菌群之间的相互作用并发现,在EM组的网络交互复杂度有所下降(图4G-F),而对照组表现出比EM组更密集、更广泛更丰富的网络交互复杂度。以上结果表明,除了菌群组成和多样性的差异外,菌群结构和菌群相互联系的复杂度之间的差异可能是导致EM群体局部炎症发生的重要原因。

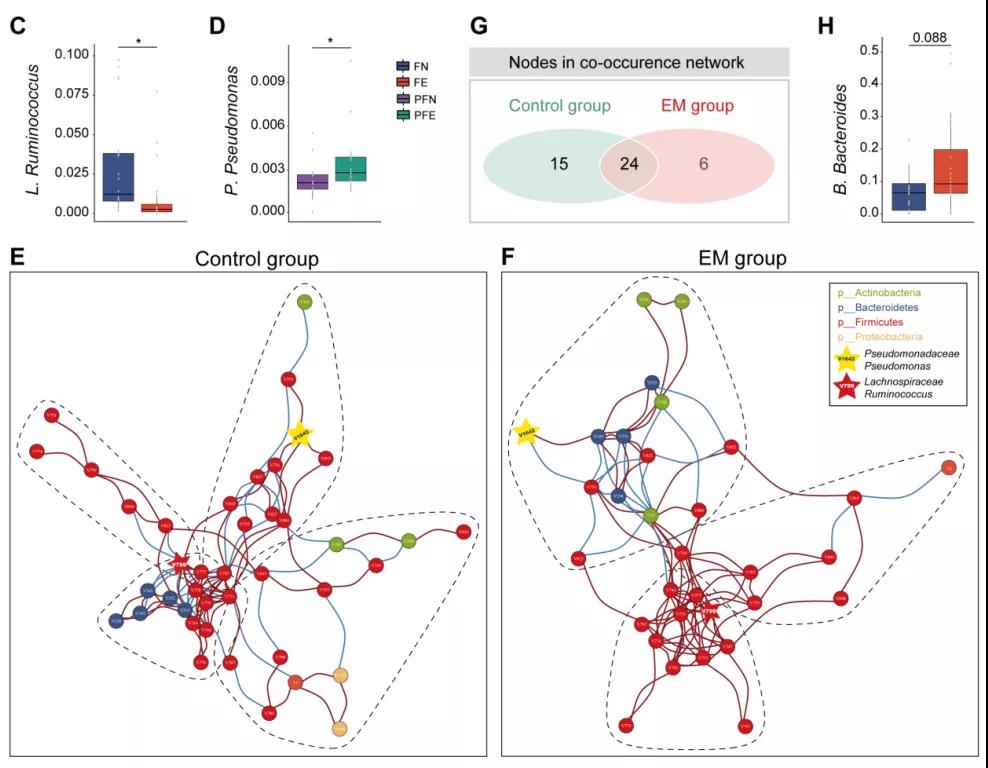
图4 不同部位菌群的生态学联系
接着,通过汇总随机森林模型重要性评分的筛选结果绘制了热图展示了在两组间的相对丰度(图5A),并基于该处展示的菌种集合分别建立了随机森林预测模型,接着利用受试者工作特征曲线(ROC)来分析机器学习算法的泛化性能。在本研究中,基于肠道菌群所建模型的AUC值达到84.0%,而宫颈粘液菌群模型AUC值仅为67.2%,腹腔冲洗液菌群模型AUC值高达88.6%。获取腹腔冲洗液的过程为有创操作,虽模型性能更优但尚不具有临床应用优势。此部分结果提示肠道菌群相对丰度对于EM具有一定的预测价值,且性能优于宫颈粘液菌群(图5B-D)。
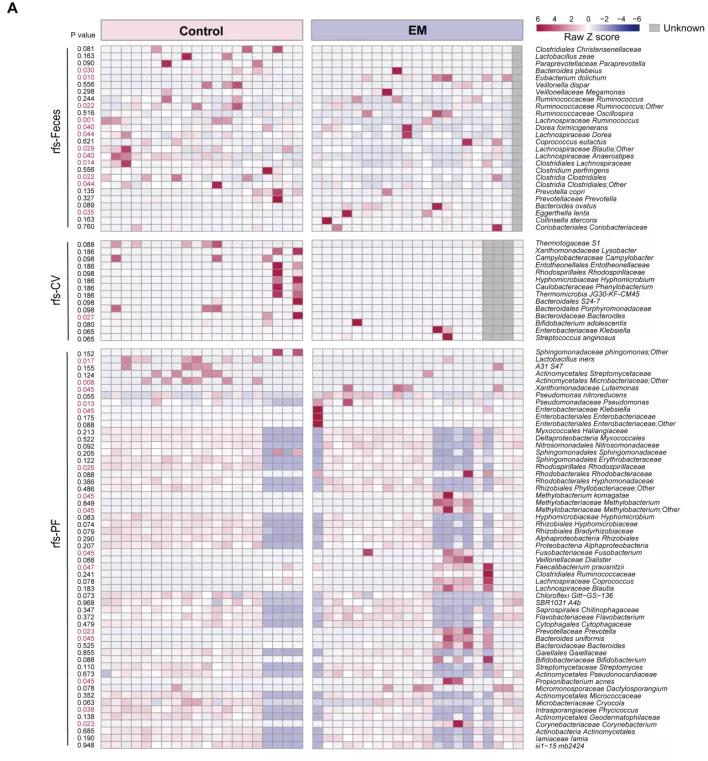
图5 基于机器学习模型筛选的菌群建立EM预测模型
总而言之,目前的研究表明,在EM人群中,肠道菌群中的有益菌相对丰度降低,盆腹腔中的有害菌相对丰度增高。最后,本研究构建了基于三个部位菌种级别相对丰度数据的机器学习模型,通过ROC曲线评估,认为肠道菌群在子宫内膜异位症的早期诊断上优于宫颈粘液菌群,对后续EM与菌群的研究具有重要指导意义。
本研究的主要完成人,第一作者黄柳菁是南方医科大学珠江医院妇产医学中心学术型硕士研究生;共同第一作者刘秉东是暨南大学第一附属医院精神医学科潘集阳教授与华南应用微生物国家重点实验室谢黎炜研究员联合培养博士研究生。本文的通讯作者为南方医科大学珠江医院妇产医学中心马颖教授,共同通讯作者为广东省科学院微生物研究所肠道微生态与健康团队PI谢黎炜研究员。
原始出处:
Liujing Huang, et al. Gut Microbiota Exceeds Cervical Microbiota for Early Diagnosis of Endometriosis. Front. Cell. Infect. Microbiol., 07 December 2021 | https://doi.org/10.3389/fcimb.2021.788836.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Cell#
30
#cellular#
49
#Biol#
46
#ERS#
33
#CRO#
36
#Bio#
35
#内膜#
30
#CEL#
34
#Micro#
41
#子宫内膜异位#
30