重磅!日本科学家首次利用皮肤细胞恢复病人视力
2016-05-16 佚名 生物谷
日本研究人员报道了他们首次成功地将来自一名女性患者皮肤细胞经重编后产生的诱导性多能干细胞(induced pluripotent stem cell, iPSC)移植到在她自己的眼睛中,最终部分地恢复她失去的视力。

日本研究人员报道了他们首次成功地将来自一名女性患者皮肤细胞经重编后产生的诱导性多能干细胞(induced pluripotent stem cell, iPSC)移植到在她自己的眼睛中,最终部分地恢复她失去的视力。他们在美国西雅图举行的2016年视觉与眼科学研究协会(Association for Research in Vision and Ophthalmology, ARVO)年度会议上报告了他们的研究结果。
这名患者是一名70岁的确诊患上年龄相关性黄斑变性(AMD)---老年人视力受损的主要病因---的老太太。作为一项初步研究的一部分,她从2014年接受这项实验性治疗。如今,在移植发生后将近2年,这些研究人员分享了他们的研究结果。
这些研究人员从这名老太太的手臂上获取一小块皮肤样品(直径4mm),然后对其中的皮肤细胞进行基因修饰,高效地将它们转化为iPSC。
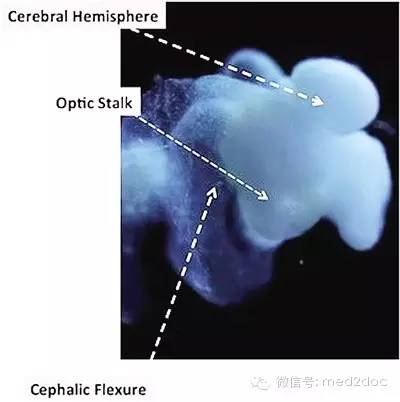
作为一种多能性干细胞,iPSC能够产生体内几乎任何一种类型组织,这就是从手臂中获取的皮肤细胞能够改为产生视网膜组织的原因。
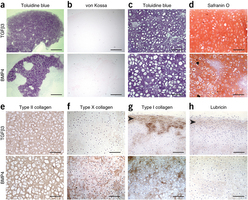
一旦iPSC经诱导产生视网膜色素上皮细胞(retinal pigment epithelium, RPE),在实验室中进行培养后,它们形成一层超薄的片状组织,然后将这种片状组织移植这名患者的视网膜后面。
2014年,项目主管、日本理化学研究所发育生物学中心科学家Masayo Takahashi说,“我为这项移植手术没有产生副作用感到非常高兴。然而,这只是将iPSC用于再生医学的第一步。但是它点燃了我继续探索的决心,直到这种治疗方法可被用于治疗很多患者。”
尽管这仍然是这种实验性治疗的初期阶段,但是迄今为止,这些结果是大有希望的。
研究人员之前一直推迟披露他们的研究结果,直到他们如今检测到这名病人的病情好转,并且检测这些修饰的细胞如何成功地持续存活,但是他们也只是报道这些移植的细胞能够存活一年多的时间,而且没有任何不良反应,这导致这名病人的视力略有改善。
研究人员在本周的一项声明中说,“在一年半的时间内,这种移植的RPE片状组织能够很好地存活下来,而且没有迹象表明存在免疫排斥,也没有意外的不良增殖,从而实现了这项初步研究的目的。”
去年,这名病人告诉《日本时报》,“我很高兴,我能够接受这种治疗。我感觉我的视线变得明亮和扩大。”
尽管这并没有完全恢复这名病人的视力,但是这项研究代表着iPSC应用向前迈出重要一步---科学家们认为iPSC可能被用来治疗很多疾病,如帕金森病和阿尔茨海默病,而不仅仅是视力问题。
许多其他研究也在给出利用干细胞治疗恢复视力取得的良好结果。今年早些时候,中国和美国科学家能够通过操纵干细胞中的蛋白水平改善白内障婴儿的视力。
更值得一提的是,美国巴尔的摩市的一名已失明5年多的女性在从将她的骨髓中提取出的干细胞注射到她的眼睛中后,恢复了她的一些视力。尽管这种特定的治疗方法仍然存在很多问题,不可否认的是,干细胞研究是一个非常令人兴奋的研究领域。
原始出处:
Japanese scientists have used skin cells to restore a patient's vision for the first time
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#本科#
40
B牛
46
#日本#
28
#重磅#
34
#皮肤细胞#
0
牛逼
138