Ophthalmologica:玻璃体腔内注射曲安奈德与白内障手术联合治疗效果评估
2018-04-16 cuiguizhong MedSci原创
日本东京女子医科大学东京医学中心眼科的Nunome T近日在Ophthalmologica发表了一篇文章,他们在抗血管内皮生长因子(抗VEGF)治疗的糖尿病性黄斑水肿(DME)患者中,评估玻璃体内注射曲安奈德注射液(IVTA)联合白内障手术治疗方法的有效性。
日本东京女子医科大学东京医学中心眼科的Nunome T近日在Ophthalmologica发表了一篇文章,他们在抗血管内皮生长因子(抗VEGF)治疗的糖尿病性黄斑水肿(DME)患者中,评估玻璃体内注射曲安奈德注射液(IVTA)联合白内障手术治疗方法的有效性。
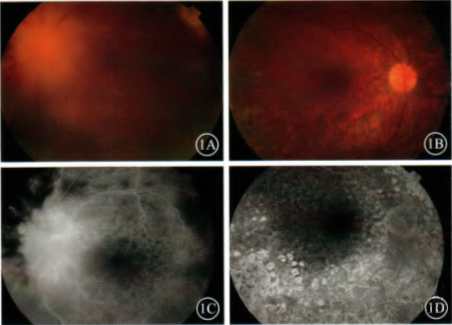
研究群体为患有屈光抗VEGF治疗的DME患者(年龄70.5±6.2岁),对其29只眼进行IVTA注射并联合白内障手术治疗。在治疗后1、4、12和24周评估视力、中心视网膜厚度(CRT)和视网膜中央敏感性。

结果发现,在治疗后24周,视力从0.49±0.30logMAR单位显着改善至0.35±0.33logMAR单位(p <0.05;重复ANOVA)。治疗后12周,CRT从435.1±112.3μm显着下降至350.8±123.3μm(p <0.05)。治疗后4周,视网膜敏感度阈值从18.2±4.3 dB显着改善至20.4±3.8 dB(p <0.05)。
因此,他们认为,IVTA联合白内障手术对患有抗VEGF治疗的DME屈光度的眼睛是有效的治疗方案。
原文出处:
Nunome, T., et al., Short-Term Results of Intravitreal Triamcinolone Acetonide Combined with Cataract Surgery for Diabetic Macular Edema in Japan: In the Era of Anti-Vascular Endothelial Growth Factor Therapy. Ophthalmologica, 2018.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#治疗效果#
30
#腔内注射#
42
#曲安奈德#
50
#效果评估#
38
好
69
学习了感谢分享
67
#联合治疗#
35
#玻璃体#
30
#白内障手术#
43
#THA#
23