PLoS One:外泌体lncRNA GAS5调节动脉粥样硬化中巨噬细胞和血管内皮细胞的凋亡
2017-10-21 MedSci MedSci原创
目前普遍认为动脉粥样硬化是血管壁的慢性脂质引起的炎症。氧化低密度脂蛋白(oxLDL)驱动涉及巨噬细胞和内皮细胞(ECs)的动脉粥样化形成的发生。本研究既往研究发现表明,患者和动物模型收集的动脉粥样硬化斑块中,长非编码RNA生长停滞特异性5(lncRNA GAS5)的表达明显增加。本研究中,研究发现敲除lncRNA GAS5可降低oxLDL处理的THP-1细胞的凋亡。相反,oxLDL刺激后,lncR
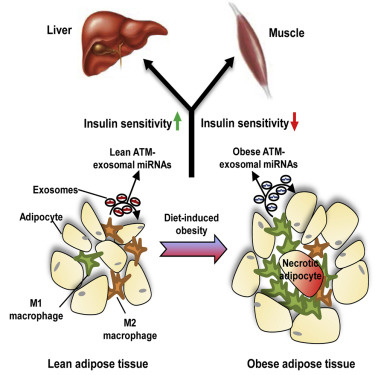
目前普遍认为动脉粥样硬化是血管壁的慢性脂质引起的炎症。氧化低密度脂蛋白(oxLDL)驱动涉及巨噬细胞和内皮细胞(ECs)的动脉粥样化形成的发生。本研究既往研究发现表明,患者和动物模型收集的动脉粥样硬化斑块中,长非编码RNA生长停滞特异性5(lncRNA GAS5)的表达明显增加。
本研究中,研究发现敲除lncRNA GAS5可降低oxLDL处理的THP-1细胞的凋亡。相反,oxLDL刺激后,lncRNA GAS5的过表达明显上调了THP-1细胞的凋亡。包括Caspase在内的凋亡因子的表达随着lncRNA GAS5的水平而改变。此外,oxLDL刺激后,THP-1来源外泌体中发现lncRNA GAS5。来源于外泌体lncRNA GAS5-过表达THP-1细胞在摄取这些外泌体后增强血管内皮细胞的凋亡。然而,敲除lncRNA GAS5的THP-1细胞的外泌体可抑制内皮细胞凋亡。
总之,这些发现揭示了lncRNA GAS5在动脉粥样硬化形成中的功能,通过外泌体调节巨噬细胞和内皮细胞的凋亡,并表明抑制lncRNA GAS5可能是治疗动脉粥样硬化的有效途径。
原始出处:
Lei Chen, Wenjin Yang, et a., Exosomal lncRNA GAS5 regulates the apoptosis of macrophages and vascular endothelial cells in atherosclerosis.PLoS One. 2017; 12(9): e0185406. Published online 2017 Sep 25. doi: 10.1371/journal.pone.0185406
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CRN#
29
#GAS#
37
#血管内皮细胞#
34
#Plos one#
28
#粥样硬化#
28
#lncRNA#
30
学习一下知识了
80
很好很好很好
71
目前普遍认为动脉粥样硬化是血管壁的慢性脂质引起的炎症.氧化低密度脂蛋白(oxLDL)驱动涉及巨噬细胞和内皮细胞(ECs)的动脉粥样化形成的发生.本研究既往研究发现表明.患者和动物模型收集的动脉粥样硬化斑块中.长非编码RNA生长停滞特异性5(lncRNAGAS5)的表达明显增加.
64