Heart:IABP可改善高危再灌注治疗患者远期生存
2013-07-30 高晓方 译 cmt
中国和美国一项联合荟萃分析表明,在接受高危再灌注治疗的患者中,辅助主动脉内球囊反搏(IABP)应用可改善远期生存率。论文于7月25日在线发表于《心脏》(Heart)。 研究者对Pubmed、Cochrane图书馆和Clinicaltrials.gov数据库进行了检索,并纳入了在高危再灌注治疗患者中对比IABP和非IABP的随机临床事件。主要转归指标为早期(30天)和远期(≥6个月)死亡率。 结
中国和美国一项联合荟萃分析表明,在接受高危再灌注治疗的患者中,辅助主动脉内球囊反搏(IABP)应用可改善远期生存率。论文于7月25日在线发表于《心脏》(Heart)。
研究者对Pubmed、Cochrane图书馆和Clinicaltrials.gov数据库进行了检索,并纳入了在高危再灌注治疗患者中对比IABP和非IABP的随机临床事件。主要转归指标为早期(30天)和远期(≥6个月)死亡率。
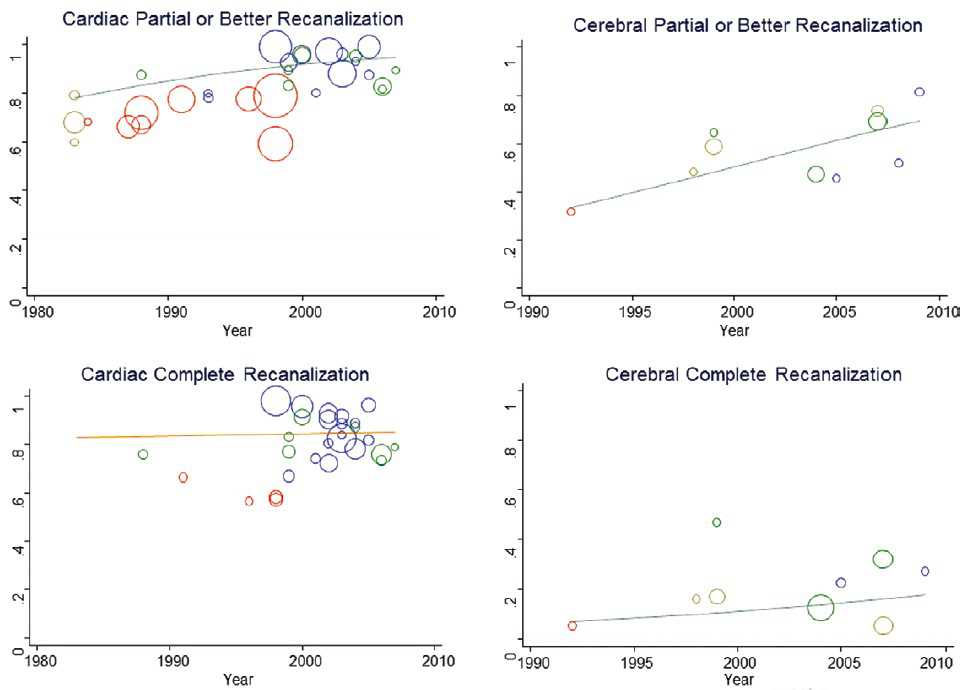
结果显示,共有涉及2037例高危患者的10项随机试验符合纳入标准。IABP组和非IABP组的早期死亡率无显著差异(OR 0.79)。然而,IABP组的远期死亡率显著降低(OR 0.63),并且在接受经皮冠脉介入治疗的亚组患者中上述效应更为显著(OR 0.55)。进一步分析显示,IABP应用与30天再缺血率(OR 0.62)以及再缺血和心衰事件复合终点(OR 0.75)风险降低相关。未观察到显著异质性。

Chen S, Yin Y, Ling Z, Krucoff MW.Short and long term effect of adjunctive intra-aortic balloon pump use for patients undergoing high risk reperfusion therapy: a meta-analysis of 10 international randomised trials.Heart. 2013 Jul 25. [Epub ahead of print]
- PMID:
- 23886602
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#ART#
21
#再灌注治疗#
47
#HEART#
28
#IABP#
28
#ABP#
24