BMC Ophthalmol:眼周基底细胞癌的5年观察结果
2022-09-08 医路坦克 MedSci原创
基底细胞癌(BCC)是一种非黑色素瘤皮肤癌类型,本研究的主要目的是回顾丹麦南部地区Vejle医院眼科手术切除眼周基底细胞癌5年的结果。回顾肿瘤病理、手术过程、并发症发生率和总体结果。
基底细胞癌(BCC)是一种非黑色素瘤皮肤癌类型,也是丹麦最常见的皮肤癌类型。根据丹麦癌症登记处的数据,2019年登记了14657例新病例。丹麦BCC的总体发病率在女性和男性中大致相似,并随着年龄的增长而增加。因此,随着预期寿命的增加,诊断为基底细胞癌并需要治疗的患者数量预计将在未来几年增加。
大约80%的BCC病例是在颈面部区域内诊断的。尽管大多数眼周肿瘤是良性的,但基底细胞癌是最常见的恶性眼周肿瘤,10–16%的基底细胞癌发生在眼睑。最常见的组织学亚型是结节性和浅表性基底细胞癌,其侵袭性较低。形态型、浸润型和小结节亚型较为罕见,但由于深层和不规则浸润的发生率较高,其本质上更具侵袭性,这可能导致不完全切除和更高的复发风险。尽管大多数BCC可分为特定的亚型,但混合模式并不罕见。
基底细胞癌很少转移,但生长模式可能具有高度破坏性,并导致严重的组织缺陷,导致严重的发病率,尤其是位于眼周时。在眼周区域有足够边缘的基底细胞癌的手术切除可能具有挑战性。保护眼睑功能和皮肤以保护视力对于获得最佳效果至关重要。除此之外,获得可接受的美容效果是另一个需要克服的挑战
本研究的主要目的是回顾丹麦南部地区Vejle医院眼科手术切除眼周基底细胞癌5年的结果。回顾肿瘤病理、手术过程、并发症发生率和总体结果。
方法:回顾2016年1月至2020年12月期间接受眼周基底细胞癌手术的所有患者的病历。所有肿瘤均切除,边缘超过临床上明显的肿瘤切除范围3mm,并通过冰冻切片组织学检查进行分析。随后对石蜡切片进行最终组织病理学诊断。记录患者年龄、性别、切除日期、既往癌症史、转诊单位和随访时间。此外,还记录了从活检和切除中确定的组织学亚型、病变位置、病变直径、首次手术后的游离边缘、泪点受累、重建技术和并发症。
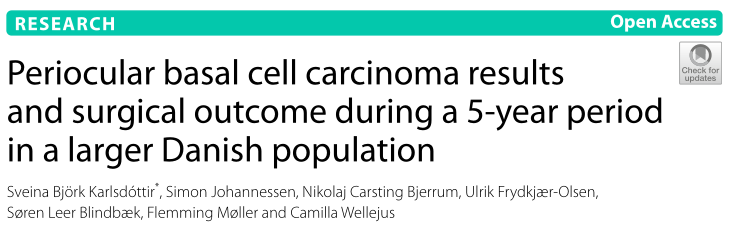
按性别和年份分列的眼周BCC数量
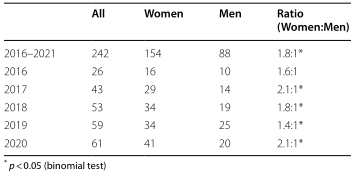
转介单位
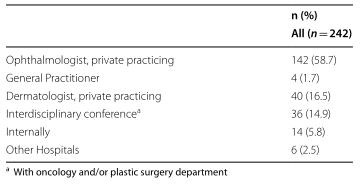
肿瘤位置
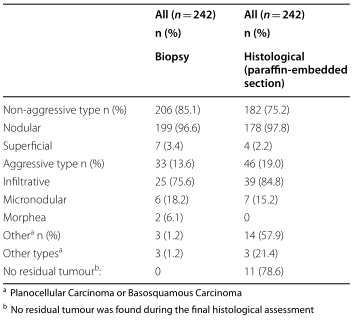
组织学亚型
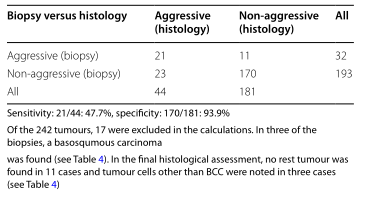
活检敏感性和特异性

并发症
结果:共记录了237例患者的242次手术切除。平均年龄为69.7±12.6岁,女性显著高于男性(1.8:1,p<0.0001,二项检验)。平均肿瘤直径为4.29毫米(范围0.5-20毫米)。最常见的部位和组织学亚型分别为下眼睑和结节性基底细胞癌(64.9%和74.0%)。在17.4%的患者中,冷冻切片组织学上的初始切除边缘没有肿瘤细胞,与非侵袭性BCC亚型(结节性和浅表性)相比,在生长模式(形态、浸润性和微结节特征)方面被认为具有侵袭性的BCC亚类型的风险显著更大(p=0.002,X2)。在239例(98.8%)患者中,最终组织病理学检查后发现基底细胞癌被彻底切除。活检中鉴别眼周基底细胞癌侵袭性亚型的敏感性为47.7%。5年期间未发现复发。
结论:本研究表明,诊断为眼周基底细胞癌的女性多于男性。对所有患者进行的初始活检低估了几乎一半病例中BCC的侵袭性,而与非侵袭性亚型相比,侵袭性BCC亚型在冷冻切片后更可能需要进一步切除。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#细胞癌#
51
#基底细胞#
48
#BMC#
42
#THA#
50