Chin Circ J:河北医大二院学者称,急诊PCI冠脉内注射依替巴肽可改善冠脉微循环
2017-08-08 许菁 中国循环杂志
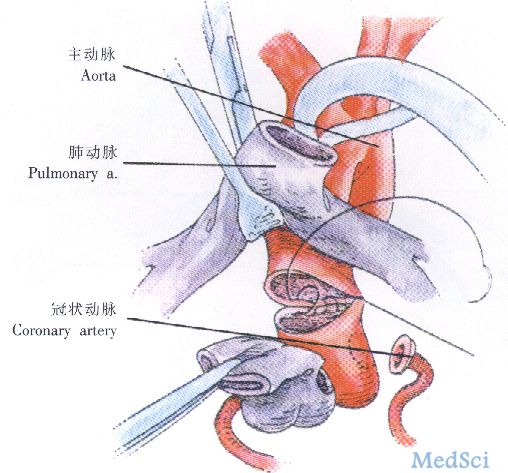
河北医科大学第二医院傅向华、薛岭等发表研究称,在STAMI患者行急诊经皮冠状动脉介入治疗(PCI)时,冠状动脉内应用依替巴肽可有效改善冠状动脉血流,增加心肌灌注,明显改善患者心功能。
河北医科大学第二医院傅向华、薛岭等发表研究称,在STAMI患者行急诊经皮冠状动脉介入治疗(PCI)时,冠状动脉内应用依替巴肽可有效改善冠状动脉血流,增加心肌灌注,明显改善患者心功能。
而且不增加大出血风险,并且随访24周,不增加MACE发生率。
本研究中,依替巴肽对微循环灌注的影响显着,与对照组比,依替巴肽组在PCI术后TIMI血流3级比例(72.5% vs 92.5%)及TIMI心肌灌注3级比例(70.0% vs 90.0%)均显着升高。
此外,依替巴肽组术后及停药后2 h血小板聚集率均较术前有显着性降低,且较对照组同时段降低。
同时在AMI后1周时依替巴肽组在硝酸甘油介入后缺血范围积分、缺血程度积分均较对照组降低,说明依替巴肽组较对照组心肌不可逆损伤减少,存活心肌面积增加。
依替巴肽组术后24周左心室舒张末直径及左心室射血分数较术后1周有显着性改善,且均优于对照组。
本研究中依替巴肽组小出血事件7例,无脑出血等大出血事件发生,对照组小出血事件3例,未见其他出血。
研究纳入急诊PCI的ST段抬高型AMI(STAMI)患者80例,随机分为依替巴肽组40例和对照组40例。
原始出处:薛玲,吴伟利,贾小倩,等.冠状动脉内应用依替巴肽对急性心肌梗死患者冠状动脉无复流和心肌灌注的影响. 中国循环杂志, 2016, 31: 862.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#微循环#
40
#急诊PCI#
35
学习
44
学习
44
学习了谢谢分享!!
38
好!
53
学习了谢谢分享!!!
42
学习一下很不错
17
非常好的文章,学习了,很受益
19
本研究中,依替巴肽对微循环灌注的影响显着,与对照组比,依替巴肽组在PCI术后TIMI血流3级比例(72.5%vs92.5%)及TIMI心肌灌注3级比例(70.0%vs90.0%)均显着升高。
16