Lancet Oncol:直肠癌术前放疗后氟尿嘧啶辅助化疗无生存优势
2014-03-10 MedSci Lancet Oncol
欧洲癌症治疗研究组织(EORTC)22921研究发现直肠癌术前放疗后氟尿嘧啶辅助化疗无生存优势。这项随机对照研究在T3或T4可切除的直肠癌患者中,观察到术前放疗组与术前放化疗组相比、术后辅助化疗组与监测组相比10年OS率(P值分别为0.91和0.32)和DFS率(P值分别为0.38和0.29)均无显著差异。单纯放疗组(252例)、新辅助放化疗组、术前放疗继辅助化疗组、新辅助放化疗继辅助化疗
欧洲癌症治疗研究组织EORTC 22921研究发现,经过了5年的随访,对于直肠癌患者术前放疗后氟尿嘧啶辅助化疗无显著生存优势。但Kaplan-Meier曲线却有不同,暗示可能推迟受益。该研究在线发表于1月17日的Lancet Oncol。【原文下载】
这项随机对照研究对T3或T4可切除的直肠癌患者中,观察到术前放疗组与术前放化疗组相比、术后辅助化疗组与监测组相比10年OS率(P值分别为0.91和0.32)和DFS率(P值分别为0.38和0.29)均无显著差异。
表1:治疗组和辅助治疗的病人情况
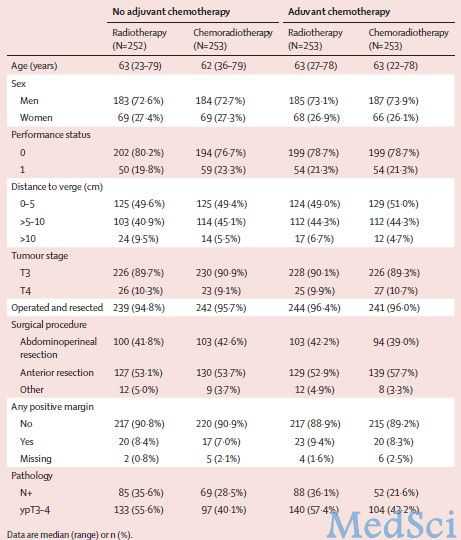
单纯放疗组(252例)、新辅助放化疗组、术前放疗继辅助化疗组、新辅助放化疗继辅助化疗组(均253例)10年局部复发累积发生率分别为22.4%、11.8%、14.5%和11.7%(P=0.0017),四组间远处转移累积发生率(P=0.52)和长期副作用无显著差异(P=0.22)。
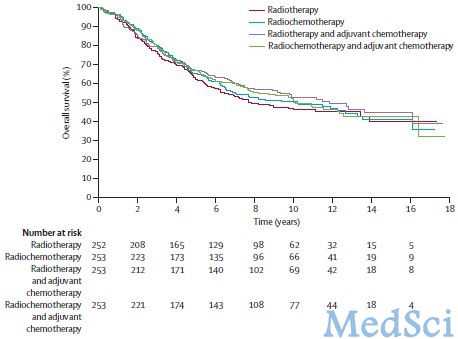
图1:各治疗方法的总体生存率对比

图1:各治疗方法的无病生存率对比
研究者表示,直肠癌术前放疗后氟尿嘧啶辅助化疗对无病生存和总生存期没有影响,其实验结果不支持术前放疗后辅助化疗手段或不采取任何化疗手段。有必要寻找新的治疗策略。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#生存优势#
22
#Oncol#
33
#Lancet#
20
#氟尿嘧啶#
32