JAMA重申:没必要——预防中风,无症状颈动脉狭窄筛查弊大于利!
2021-02-11 MedSci原创 MedSci原创
USPSTF认为对无症状人群筛查的危害大于益处,在此次2021年更新的建议中再次确认不要对无症状者做颈动脉狭窄筛查。
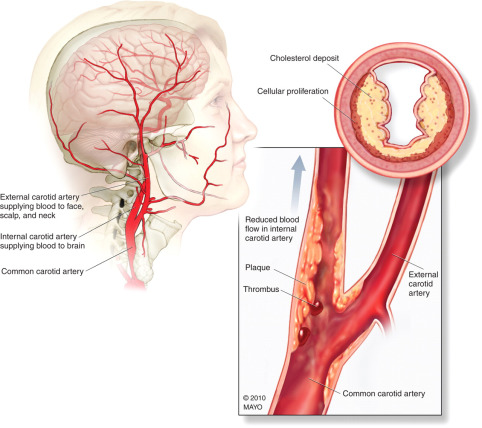
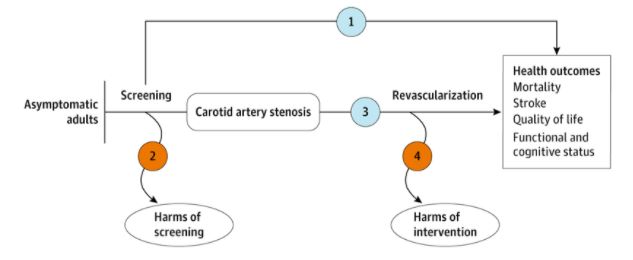
颈动脉狭窄是一个公认的卒中危险因素和心血管疾病标志物。但截止目前,尚未对颈动脉狭窄进行基于人群的筛查试验,因此临床上无症状颈动脉狭窄的最佳治疗方法仍不确定。目前可选方案主要是单独使用最佳药物治疗或与血管重建术(颈动脉内膜切除术或颈动脉支架术)联合使用以预防卒中。既往试验显示,与单独使用最佳药物疗法相比,血管内治疗长期获益较小,同时还可能带来额外的手术伤害。
自2007年以来,美国预防服务特别工作组(USPSTF)一直推荐D级证据,即反对在普通成人人群中筛查无症状的颈动脉狭窄。USPSTF认为,一般人群中无症状颈动脉狭窄导致的卒中发生率较低;同时研究显示,与药物治疗相比,手术的获益较小;此外还有轻中度的手术危害。随后,2014年该工作组的建议再次保留了上述观点。
最近,USPSTF对2014年后获得的最新研究证据进行汇总分析,发表在最新的JAMA杂志上。与上两次声明一致,该工作组建议对于没有中风、神经系统症状或短暂性脑缺血发作症状的成年人来说,不需要进行无症状颈动脉狭窄筛查。这也与美国心脏协会(AHA)/美国卒中协会(ASA)的建议相吻合。
研究人员对从2014年1月1日至2020年2月18日发表在MEDLINE、PubMed以及Cochrane上的对照试验进行了文献检索。由两位研究者独立评估了符合纳入标准的文章,并对数据进行提取与分析。同时对每个美国国家数据库或手术注册表中报告的最新综合研究进行审查。
结果共筛选了2373篇文章。符合纳入条件的研究没有证据表明直接检查无症状颈动脉狭窄筛查的益处或危害。仅两项有限的、过早终止的试验报告了颈动脉血管重建加最佳药物治疗与单纯药物治疗的比较效果,但结果不一。
其中,SPACE-2试验(n = 316)结果显示,与药物治疗相比,颈动脉内膜切除术(HR=2.82)或颈动脉支架植入术(HR=3.50)在1年后卒中或死亡的发生率无显著差异。另一项规模较小的AMTEC试验(n = 55)则报道,颈动脉内膜切除术组在中位随访3.3年时,非致命性同侧卒中或死亡的复合风险显著降低,具有统计学意义(HR=0.20)。
在一篇社论中, 肯塔基大学的Larry Goldstein教授认为,当前证据支持USPSTF重申针对无症状性颈动脉狭窄人群的筛查建议。因为无症状的颈动脉狭窄相关的中风人群归因风险估计仅为0.7%,大大低于其他中风风险因素。
研究人员随后分析了颈动脉筛查的益处与危害。
从益处方面来说:1)虽然有充分的证据表明,多普勒超声检查对检测临床相关的颈动脉狭窄具有敏感性和特异性,但是当普通人群筛查时,可能会产生假阳性结果。2)颈部听诊颈动脉杂音的准确性较差,无法检测出临床相关的颈动脉狭窄。也没有足够的直接证据表明,筛查无症状的颈动脉狭窄可以降低不良健康结局(例如中风,死亡率)。
从危害来说:1)目前虽然没有足够的直接证据表明,筛查无症状颈动脉狭窄会造成危害,但与目前的治疗相比,用手术或基于导管的方法治疗无症状患者,在减少不良健康结局方面没有或只有很小的益处。2)用于确诊的检测和干预措施(如计算机断层扫描、磁共振成像和侵入性血管造影等)会造成额外危害。
因此,根据USPSTF的评估,无症状颈动脉狭窄的筛查和治疗的总体危害程度为轻中度。
综上,USPSTF认为对无症状人群筛查的危害大于益处,在此次2021年更新的建议中再次确认不要对无症状者做颈动脉狭窄筛查。
参考文献:
Guirguis-Blake JM, et al. Screening for Asymptomatic Carotid Artery Stenosis in the General Population: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2021 Feb 2;325(5):487-489. doi: 10.1001/jama.2020.20364.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








精彩评论,需要您登录查看
66
#颈动脉#
31
#无症状颈动脉狭窄#
49
别看见了狭窄就给人家切开或者放支架。。。。
63
希望能看到中国的前瞻性研究数据。
77
结合实际
109
好文章
107
#无症状#
32
#动脉狭窄#
32
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
25