Hypertension:动脉僵硬度越高,大脑血管储备越低!
2018-06-19 MedSci MedSci原创
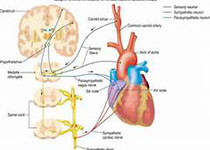
主动脉僵硬度和脉压增高与人类脑血管重构、白质微结构减少以及衰老相关的认知表现相关。但是,尚不明确主动脉僵硬度和脉压是否与老年人基地总动脉脑血流量(CBF)减少和脑血管储备相关。研究人员招募205位成年人(19-87岁;平均±SE:30.6±1.3岁),用[15O]水大脑正电子发射断层扫描定量全脑CBF。评估老年亚群(24人;70.0±2.0岁)的动脉僵硬度(颈股动脉脉搏速度)和脑血管储备(静脉点滴
研究人员招募205位成年人(19-87岁;平均±SE:30.6±1.3岁),用[15O]水大脑正电子发射断层扫描定量全脑CBF。评估老年亚群(24人;70.0±2.0岁)的动脉僵硬度(颈股动脉脉搏速度)和脑血管储备(静脉点滴乙酰脞胺后全脑CBF变化)。在整个队列中,老年人的全脑CBF低于年轻成年人的(51.0±0.30 vs 47.4±0.03mL/min·100mL;p<0.001),老年男性和女性之间没有差异(p=0.63)。在老年人中,颈股动脉脉搏速度越大,脑血管储备越少(r=-0.68;p=0.001),但全脑CBF不受影响(γ=0.13;p=0.60)。手臂脉搏压与脑血管储备多少无关(γ=-0.37;p=0.159)。
本研究结果表明,随着不断的衰老,主动脉僵硬增加或许在一定程度上会导致大脑受刺激时增加血流的能力受损。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TENS#
24
#PE#
20
#Hypertension#
33
#动脉僵硬#
35
#动脉僵硬度#
36