Stroke:e-ASPECTS评分的临床价值
2018-07-22 杨中华 脑血管病及重症文献导读
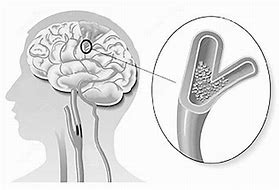
平扫CT(Noncontrast enhanced computerized tomography,NCCT)是急性卒中最广泛采用的影像学诊断方法。除了费用低廉、快速以外,排除颅内出血和颅内占位的可靠诊断工具,NCCT还能为再灌注治疗的提供辅助决策。
平扫CT(Noncontrast enhanced computerized tomography,NCCT)是急性卒中最广泛采用的影像学诊断方法。除了费用低廉、快速以外,排除颅内出血和颅内占位的可靠诊断工具,NCCT还能为再灌注治疗的提供辅助决策。
ASPECTS(Alberta Stroke Program Early CT Score)评分用来判断幕上MCA供血区(10个区域)的缺血性改变,是一种简单的定量工具。电子ASPECTS评分(e-ASPECTS)是一种自动影像分析软件,对怀疑为急性缺血性卒中的患者提供临床决策。基于机械学习法则,e-ASPECTS能够对NCCT的层面进行快速和标准化自动分析,其对早期缺血性改变的识别能力不次于有经验的神经影像学专家。此外,e-ASPECTS还能预测大动脉闭塞患者采用机械性取栓治疗后的死亡和残疾。然而,e-ASPECTS评分的验证性研究都是小型筛选的病例研究。
2018年6月来自德国的Simon Nagel等在Stroke上公布了他们的研究结果,他们利用ENCHANTED试验患者的NCCT数据,目的在用评价e-ASPECTS评分对急性缺血性卒中静脉溶栓患者的临床价值。
ENCHANTED试验是探讨小剂量rtPA和标准剂量rtPA不同的随机多中心对照研究。研究者把该研究中基线NCCT质量不佳和层厚超过6mm的患者排除在外。
共2426个可用的CT影像,1480(61%)纳入到e-ASPECTS评分分析中(平均9分[四分位距,8-10],77% with good [range, 8–10] scores)。较低e-ASPECTS评分(每降低1个点)与基线NIHSS评分增加(r,-0.31;P < 0.0001)和90天不良预后(mRS,2-6)(r,-0.27;P < 0.001)显着相关。90天mRS 2-6分的调整OR为0.91(95% CI,0.85-0.97),90天mRS 3-6分的调整OR为0.89(95% CI,0.83 - 0.95),90天mRS 6分的调整OR为0.86(95% CI,0.79 - 0.95);症状性颅内出血的OR为0.87(0.72 - 1.05)。
最终作者认为e-ASPECTS评分与基线神经功能严重性相关,能够独立预测急性缺血性卒中患者的功能恢复和不良结局。
原始出处:Nagel S1, Wang X2, Carcel C, et al. Clinical Utility of Electronic Alberta Stroke Program Early Computed Tomography Score Software in the ENCHANTED Trial Database. Stroke. 2018 Jun;49(6):1407-1411.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#临床价值#
48
#PE#
37
#ASPECTS#
45
#CTS#
35