Lancet Oncol:Buparlisib联合内分泌治疗HR+/HER2-患者带来生存改善
2017-06-12 佚名 肿瘤资讯
激素受体阳性(HR+)乳腺癌是最常见的乳腺癌类型,内分泌治疗是HR+乳腺癌治疗的基石。在HR+乳腺癌患者中,PI3KCA突变可能阶段内分泌耐药。早期研究提示Buparlisib联合氟维司群用于内分泌耐药的HR+/HER2-患者,耐受性可,可见初步疗效。III期BELLE-2研究进一步评估了这一方案的疗效价值。
激素受体阳性(HR+)乳腺癌是最常见的乳腺癌类型,内分泌治疗是HR+乳腺癌治疗的基石。在HR+乳腺癌患者中,PI3KCA突变可能阶段内分泌耐药。早期研究提示Buparlisib联合氟维司群用于内分泌耐药的HR+/HER2-患者,耐受性可,可见初步疗效。III期BELLE-2研究进一步评估了这一方案的疗效价值。
背景
近年来的研究显示,HR+乳腺癌是一类异质性很大的肿瘤,不同的基因特征影响其治疗的疗效,但不同肿瘤独特的基因突变谱,也提示其可能从靶向治疗中获益。在HR+乳腺癌患者中,PI3KCA(编码PI3K激酶的p110α异构体)突变非常常见,其可能介导内分泌治疗耐药,因此对于内分泌治疗进展的患者,靶向PI3K可能为潜在的治疗策略。
早期试验中,PI3K抑制剂单独用于内分泌耐药患者,活性较低。后续研究发现,耐药患者中还同时存在ESR1突变等,增强ER通路的活化,联合应用PI3K抑制剂和ER拮抗剂氟维司群,可产生协同抗肿瘤作用。III期研究BOLERO-2显示,mTOR抑制剂依维莫司联合依西美坦用于内分泌治疗进展后的HR+/HER2-晚期乳腺癌显示出很好的疗效,然而mTOR的激活机制非常复杂,仅部分依赖于PI3K。Buparlisib(BKM120)是口服泛-PI3K抑制剂,可以靶向I型PI3K的4个异构体(α,β,γ,δ)。动物实验显示Buparlisib联合氟维司群可显着抑制HR+乳腺癌生长。I期研究也显示这一组合方案,耐受性好,且看到了初步疗效。III期研究BELLE-2旨在绝经后AI耐药的HR+/HER2-晚期乳腺癌中,评估Buparlisib联合氟维司群的疗效和安全性,并探索PI3K通路激活状态能否作为疗效预测指标。
方法
这一研究入组了绝经后,年龄≥18岁,组织学或细胞学确认的HR+/HER2-乳腺癌,且能够获取足够的肿瘤组织。患者为不可手术的局部晚期或转移性疾病。接受辅助AI治疗进展12个月,或转移性或晚期疾病时接受AI治疗,进展1个月内。只要患者符合AI原发耐药的定义,允许患者既往接受过多线的内分泌治疗。在AI耐药前后接受过其他的抗肿瘤治疗的患者也可以入组。最近一次组织活检的结果确认HR+/HER2-。
入组患者随机1:1分配接受氟维司群+buparlisib或氟维司群+安慰剂,分层因素包括肿瘤组织PI3K通路活化状态(激活 vs 未激活 vs 未知),和内脏转移状态(有 vs 无)。所有入组患者首先开始14天的治疗准备期,并在第1周期第1天接受氟维司群500mg治疗。在此期间,中心实验室检测PI3K的通路活化状态(采用Sanger测序PIK3CA基因和IHC检测PTEN表达)。据检测结果,患者被分为3组:PI3K通路激活(PI3KCA外显子1,7,9或20检测到任意突变;或PTEN蛋白不表达:<10%的细胞表达水平为1+,且无细胞表达>1+);PI3K通路未激活组(无PI3KCA突变,且可以检测到PTEN表达);PI3K通路激活状态未知(PIK3CA和PTEN的检测结果不能解读)。所有患者在第1周期第1天和第15天;及之后每周期的第1天接受氟维司群500mg治疗,28天为1个周期。患者在入组后第1个周期的第15天随机分配接受buparlisib(100 mg,每天,从第1个周期的第15天开始服药)或安慰剂治疗。所有患者持续治疗直至疾病进展,不可耐受的毒性,死亡或其他原因终止治疗。最多可以进行3次buparlisib或安慰剂的剂量调整:80mg/d持续用药;100mg/d,每周用药5天;或80mg/d,每周用药5天。
在研究发现可采用ctDNA检测患者的突变状态时,修改了研究方案,要求入组患者留取基线的血标本,之前的研究方案,患者自愿选择是否留取血标本。采用BEAMing法检测15个PIK3CA突变(外显子1,7,9,20,Arg88Gln, Arg93Trp/Gln, Lys111Glu/ Asn, Gly118Asp, Glu365Lys, Cys420Arg, Glu542Lys, Glu545Gly/Lys, Gln546Lys, and His1047Arg/Leu/Tyr)。研究主要终点为所有入组患者的PFS,主要研究队列(即PI3K激活状态已知患者)的PFS,和PI3K通路活化患者的PFS。次要研究终点为所有入组患者,主要研究队列和PI3K通路活化患者的OS。
结果
参与随机的患者1147例,buparlisib+氟维司群组576例,安慰剂+氟维司群组571例。两组的基线特征均衡。患者的中位年龄为62岁,98%的患者ECOG PS评分0-1分,678例(59%)患者合并内脏转移,>99%的患者既往接受过AI治疗,73%的患者既往接受过化疗(包括辅助阶段),分别有847例(74%)和318例(28%)的患者在转移性疾病阶段接受过内分泌治疗和化疗。
1147例患者中,372例(32%)患者PI3K通路激活,479例(42%)未激活,296例(26%)状态未知。在860例采用组织检测获知PI3KCA的患者中,276例(32%)有PIK3CA突变。在587例采用ctDNA检测PIK3CA状态的患者中,200例(34%)患者PIK3CA突变。
研究达到了主要终点,总人群中,buparlisib对比安慰剂可显着改善PFS:mPFS分别为6.9m(95%CI:6.8-7.8)和5.0m(95%CI 4.0-5.2),HR=0.70[95%CI 0.67-0.89],单侧p=0.00021,如下图1A.主要研究队列中(buparlisib组n=427;安慰剂组n=424),buparlisib对比安慰剂也能显着延长PFS(mPFS为6.8m[95%CI 5.0-7.0] vs 4.5m[3.3-5.0];HR=0.8[95%CI 0.68-0.94])。而在372例PI3K活化的患者中(buparlisib组n=188;安慰剂组n=184),根据研究设定的标准,单侧α=0.01,两组PFS无统计学差异,分别为6.8m和4.0m,HR=0.76[95%CI 0.60-0.97],单侧p=0.014,如图1B所示。
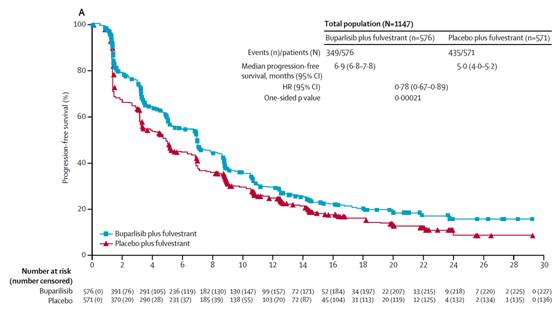
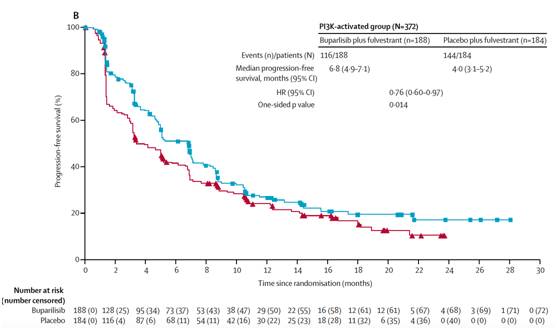
图1A.总人群的PFS比较;B. PI3K通路活化患者的PFS比较。
OS的数据还未成熟,总人群中共281例(24%)患者达到死亡终点。在总人群中,buoarlisib组和安慰剂组的ORR分别为11.8%和7.7%;临床获益率CBR分别为43?8%和42.0%。既定的探索性分析为ctDNA检测到的PIK3CA突变患者的PFS。共446例患者有配对的组织和ctDNA样本,组织和ctDNA检测的一致性为77%(342/446)。在307例组织PIK3CA野生型的患者中,243例(79%)患者ctDNA未检测到突变,64例(21%)检测到PIK3CA突变,提示肿瘤可能在治疗过程中发生进化。在采用ctDNA检测PI3KCA突变状态的患者中,buparlisib对比安慰剂可显着延长PFS,见下图2A,但在PI3KCA野生型的患者中,两组PFS无统计学差异,见图2B。


图2. 采用ctDNA检测PIK3CA突变状态患者的PFS比较。A.ct-DNA突变的患者;2B.ctDNA野生型患者。
结论和点评
这一研究提示,PI3K抑制剂联合内分泌治疗用于ctDNA检测到PI3KCA突变的绝经后内分泌耐药的HR+/HER2-患者,可以给患者带来显着的临床获益。需要后续的研究进一步探索ctDNA PI3KCA状态能否作为疗效预测标志物。因为buparlisib为泛-PI3K抑制剂,这一组合方案毒性较大,后续不再进行进一步的研究。期待后续的研究能进一步评估PI3Kα-特异性抑制剂联合方案的疗效和安全。新药层出不穷的时代,靶向药物的疗效和安全性同等重要。
原始出处:
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#分泌#
35
#buparlisib#
32
#Oncol#
38
#Lancet#
39
#uPAR#
38
#HER2-#
41