J Clin Oncol:现实残酷!- cSCCHN患者术后同步放化疗效果并不优于单独放疗
2018-03-18 慧语 肿瘤资讯
3月15日,《Journal of clinical oncology 》杂志在线发表了跨塔斯曼放射肿瘤组织(TROG)的一项随机III期临床TROG 05.01(ClinicalTrials.gov:NCT00193895)的结果,该试验旨在评估在术后放疗(CRT)中增加同步化疗是否能改善高危皮肤头颈部鳞状细胞癌(cSCCHN)患者的局部控制率。
3月15日,《Journal of clinical oncology 》杂志在线发表了跨塔斯曼放射肿瘤组织(TROG)的一项随机III期临床TROG 05.01(ClinicalTrials.gov:NCT00193895)的结果,该试验旨在评估在术后放疗(CRT)中增加同步化疗是否能改善高危皮肤头颈部鳞状细胞癌(cSCCHN)患者的局部控制率。
背景
对于高风险头颈部黏膜鳞状细胞癌(SCCHN)患者,基于铂类的术后化放疗(CRT)在局部控制(LRC),无进展生存期和总生存期(OS)方面均优于单独放疗(RT)。尽管许多研究已将术后CRT的使用外推至皮肤SCCHN(cSCCHN),尤其是在存在阳性切缘和淋巴结囊膜外扩散(ECE)的情况下。但目前并没有高级别的证据 支持CRT在此情况下的应用。因此,TROG进行了此项随机III期临床试验-称为POST研究(Postoperative Skin Trial,术后皮肤试验),以确定在术后放疗基础上加用卡铂能否改善高危cSCCHN患者的LRC。
方法
两组的治疗方案分别是60或66Gy放疗联合卡铂(CRT)和单纯放疗(RT)。主要研究终点是无局部区域复发率(FFLRR)。次要研究终点是无病生存期(DFS)和总生存期(OS)。
结果
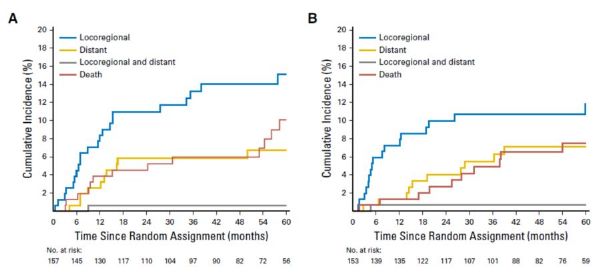
321名患者进行随机,其中310名患者接受了实际治疗:单独放疗(RT)组157例; 放化疗(CRT)组153例。 238名患者(77%)有高危淋巴结转移,59名(19%)患有高风险的原发或传播类疾病,13名(4%)同时有以上两种疾病。中位随访时间为60个月。RT组的中位剂量是60 Gy,CRT组有84%的患者完成6个周期的卡铂。 RT组2年和5年FFLRR分别为88%(95%CI,83%~93%)和83%(95%CI,77%~90%),CRT组分别为89%(95%CI,84%~94%)和87%(95%CI,81%~93%),两组的风险比HR=0.84(95%CI,0.46~1.55; P = .58,图1)。无病生存率或总生存率同样没有统计学显着差异(图2-3)。孤立性远处转移是第一次治疗后最常见的失败类型,在两组中均为7%。第一次治疗失败后各终点事件随时间的累积发生率见图4。两组患者治疗耐受性良好,未观察到联合卡铂的RT毒性增强。 3级或4级迟发毒性偶有发生。
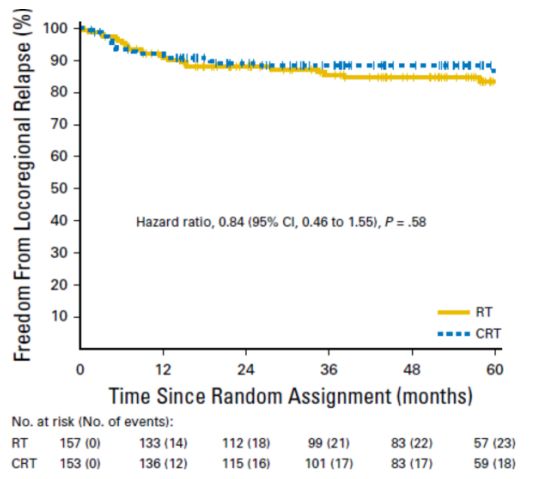
图1 RT组和CRT组的FFLRR曲线
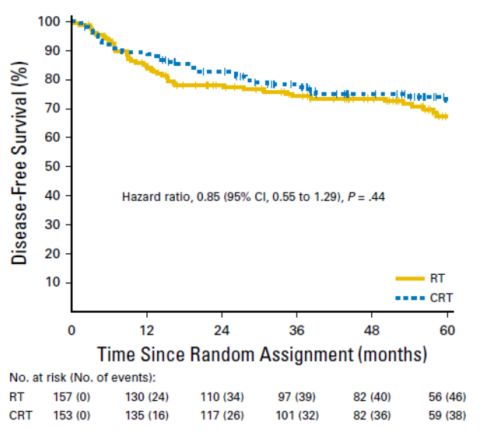
图2 RT组和CRT组的DFS曲线

图3 RT组和CRT组的OS曲线
图4 第一次治疗失败后各终点事件的随时间的累积发生率(A)RT组(B)CRT组
结论
术后放疗提供了理想的FFLRR,且每周卡铂的添加并没有观察到更多的获益。
原始出处:
Sandro Virgilio Porceddu,et al.Postoperative Concurrent Chemoradiotherapy Versus Postoperative Radiotherapy in High-Risk Cutaneous Squamous Cell Carcinoma of the Head and Neck: The Randomized Phase III TROG 05.01 Trial.J Clin Oncol.March 14, 2018
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#SCC#
28
#Oncol#
26
学习了谢谢分享!!
49
#放化疗#
36
#同步放化疗#
30
阅
48
阅
45
不错耶.学习了
52
学习了很有用不错
51
3月15日.杂志在线发表了跨塔斯曼放射肿瘤组织(TROG)的一项随机III期临床TROG05.01(ClinicalTrials.gov:NCT00193895)的结果.该试验旨在评估在术后放疗(CRT)中增加同步化疗是否能改善高危皮肤头颈部鳞状细胞癌(cSCCHN)患者的局部控制率
21