Advanced Functional Material:在培养皿中人工制造骨骼组织
2021-02-11 MedSci原创 MedSci原创
能精确还原骨骼微小结构的系统——bio-tSPL
骨科研究的艰难之处不仅在于需要创造出与真实骨组织精确匹配的人造骨组织,还需要准确还原出骨微环境,即骨骼干细胞分化起重要作用的微小结构,这对骨再生至关重要。
近日,来自美国纽约大学丹顿工程学院和纽约干细胞基金会研究所(NYSF)的研究人员在《先进功能材料》杂志上发表题为《Cost and Time Effective Lithography of Reusable Millimeter Size Bone Tissue Replicas with Sub-15 nm Feature Size on a Biocompatible Polymer》的研究论文。

在该研究中,研究人员使用生物热成像技术与热纳米凿建造了一个能精确骨微环境的系统——bio-tSPL。
在人体内,骨骼干细胞生活在胶原蛋白分子、骨蛋白和矿物质的聚集体中。骨的层次结构在微纳级别,其复杂性极大的阻碍了精细骨骼结构的复制。
bio-tSPL平台够对骨组织进行“拍照”,然后利用这张照片制作出具有确切结构的骨组织复制品,可以帮助我们制造出更有效的骨植入物,以治疗由损伤或疾病引起的骨骼缺损,为理解细胞生物学和骨病建模以及开发更先进的药物筛选平台提供了可能性。
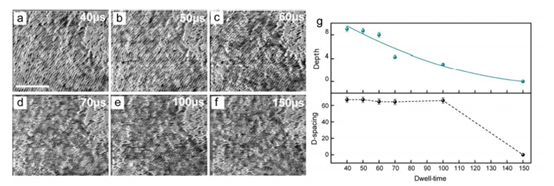
不同停留时间的tSPL热图像
bio-tSPL的时间和成本效益,以及细胞兼容性和复制骨的可重复使用性,使它成为了一个性价比和信赖度都非常高的平台,并能以前所未有的精度完美再生任何生物组织。
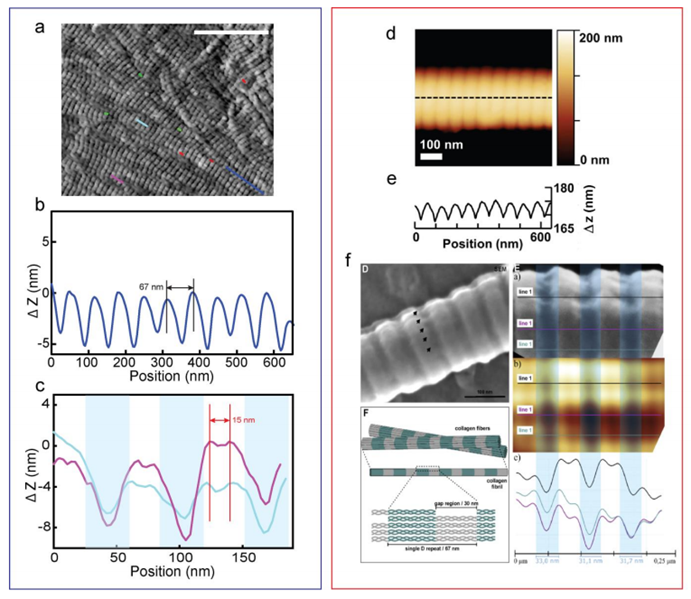 tSPL骨组织复制品(蓝框)与骨组织之间的比较(红框)
tSPL骨组织复制品(蓝框)与骨组织之间的比较(红框)
该研究的领导者之一Elisa Riedo教授表示:bio-tSPL是其实验室率先开发的一种强大的纳米加工方法。直到今天,材料的通量和生物相容性方面的限制仍然是阻止它们在生物学研究中被广泛使用的主要原因之一。bio-tSPL能够突破这些障碍并广泛的应用到生物医学领域。
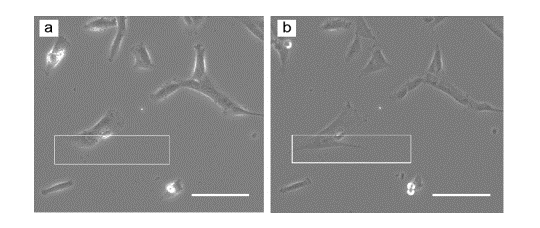
模型复制品上的细胞生长
总而言之,这项技术可能会彻底改变药物研发,帮助开发出更好的骨骼植入物和设备,开创了具有广泛研究和治疗潜力的新型干细胞应用的先驱,对于生物医学研究和应用有非凡的意义。
原始出处
Xiangyu Liu, Alessandra Zanut, Martina Sladkova‐Faure, Liyuan Xie, Marcus Weck, Xiaorui Zheng, Elisa Riedo, Giuseppe Maria Peppo. Cost and Time Effective Lithography of Reusable Millimeter Size Bone Tissue Replicas With Sub‐15 nm Feature Size on A Biocompatible Polymer. Advanced Functional Materials, 2021; 2008662 DOI: 10.1002/adfm.202008662
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Advanced#
58
#functional#
48
666
82
#function#
0
涨知识
86