Eur Heart J:多发瓣膜性心脏病患者的特征、治疗和结局
2022-05-02 MedSci原创 MedSci原创
多发性VHD较为常见,近30%的患者为左侧VHD,并与更大程度的心脏损伤相关;在6个月时,与单一VHD患者相比,多发性VHD患者出现了更高的死亡率和更多的心力衰竭病例,但手术率较低。
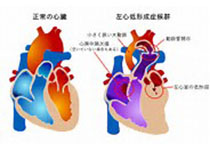
多发瓣膜性心脏病(VHD)是一种非常常见的疾病,其定义是存在至少两个心脏瓣膜相关的返流和/或狭窄性病变。在一项基于瑞典全国医院登记中心的VHD流行病学研究中,10%的瓣膜病患者为多发性VHD。在EuroHeart的第一次调查中,16.8%接受瓣膜手术的患者为多发性VHD,而根据美国胸外科医生协会数据库,11%接受瓣膜手术的患者为双瓣膜手术。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,该研究旨在评价多发性VHD患者的特点、治疗和生存情况。

在纳入了欧洲观察性VHD II调查研究的一处以上严重左侧VHD患者中,3571例患者有单侧左侧VHD (A组,70.2%),363例患者左侧有一处严重的VHD,而右侧存在中等程度的VHD(B组,7.1%)和1153名患者(22.7%)有2处以上严重VHD(左和/或三尖瓣返流,C组)。

多发性VHD (B和C组)患者更多为女性,伴有更严重的充血性心力衰竭(CHF)和更多合并症,左房容积和肺动脉压也均高于A组,射血分数低于A组(所有P≤0.01)。在住院期间,A组(36.7%,n=1312)、B组(26.7%,n=97)、C组(32.7%,n=377)的患者接受了瓣膜介入治疗(P<0.001)。即使校正了年龄、性别、体重指数和Charlson指数[风险比(HR)和95%置信区间(CI) 为1.62 (1.10-2.38) vs. B组;HR和95%置信区间(CI) 为1.72 (1.32-2.25) vs. C组],A组患者的6个月生存率优于B组或C组(所有P<0.001)。B组和C组在6个月时的CHF的人数多于A组(P<0.001)。C组死亡的相关因素为年龄、CHF和合并症(所有P<0.010)。
由此可见,多发性VHD较为常见,近30%的患者为左侧VHD,并与更大程度的心脏损伤相关;在6个月时,与单一VHD患者相比,多发性VHD患者出现了更高的死亡率和更多的心力衰竭病例,但手术率较低。
原始出处:
Christophe Tribouilloy,et al.Characteristics, management, and outcomes of patients with multiple native valvular heart disease: a substudy of the EURObservational Research Programme Valvular Heart Disease II Survey.European Heart Journal.2022.https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehac209/6576528
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#瓣膜性心脏病#
0
#瓣膜性#
49
#ART#
42
#HEART#
0
#瓣膜#
52