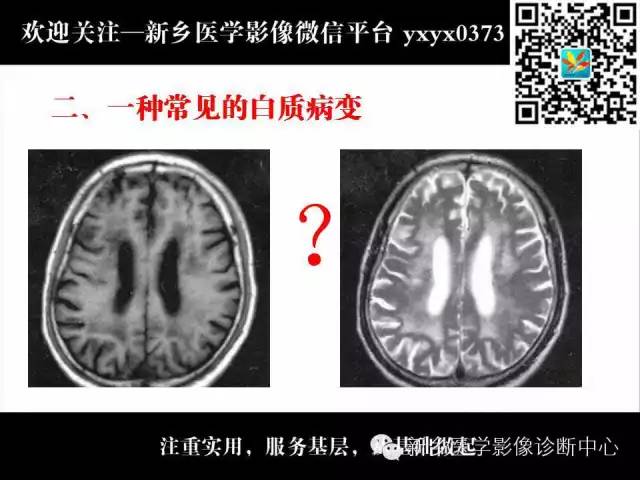
MRI多发星点高信号,白质脱髓鞘?白质疏松?脑白质变性?皮脑?让我们一起看看专家大伽如何报告的
2022-05-29 华夏影像诊断中心 华夏影像诊断中心
MRI多发星点高信号,白质脱髓鞘?白质疏松?脑白质变性?皮脑?让我们一起看看专家大伽如何报告的(内附北京协和冯逢教授观点视频)
MRI多发星点高信号,白质脱髓鞘?白质疏松?脑白质变性?皮脑?让我们一起看看专家大伽如何报告的(内附北京协和冯逢教授观点视频)






(建议直接把进度调节到36:50时间处进行观看)
(建议直接把进度调节到36:50时间处进行观看)

来源:熊猫放射
作者:花人青










小 结
-
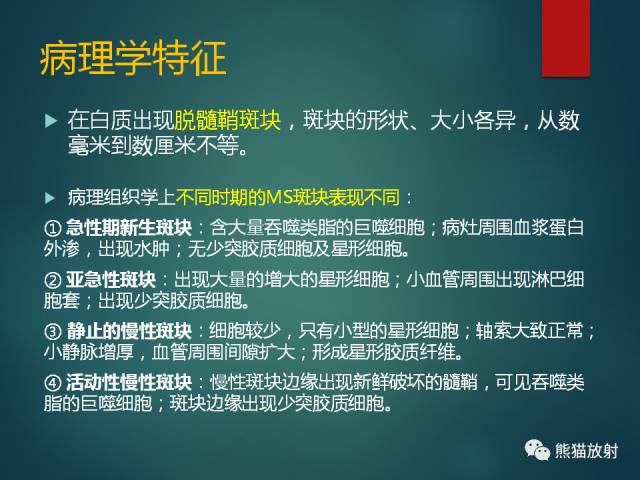
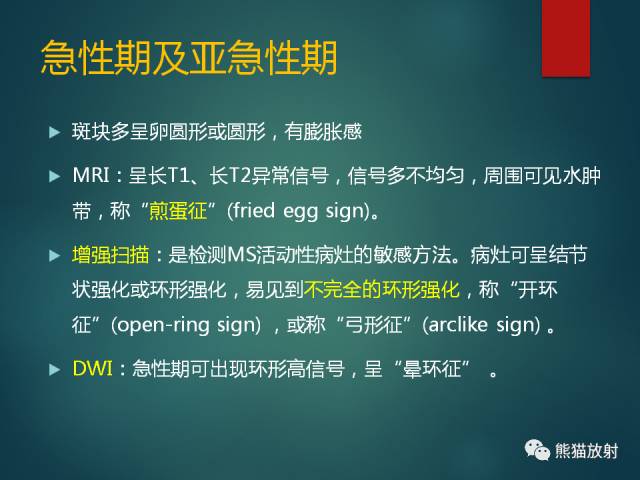
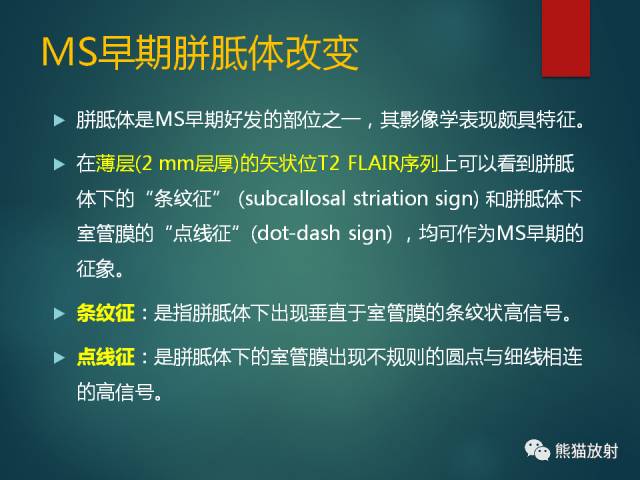
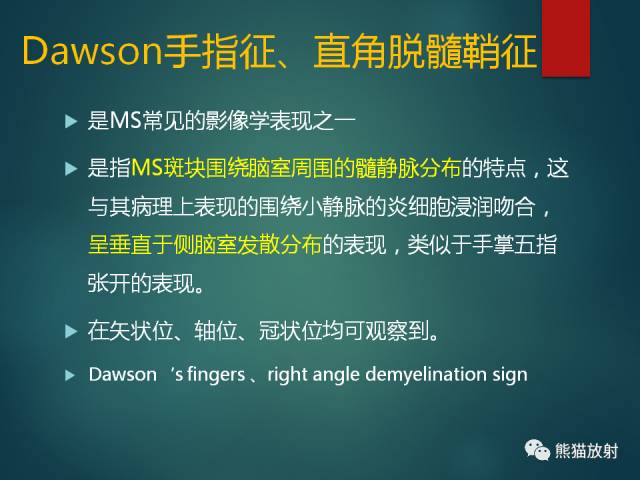
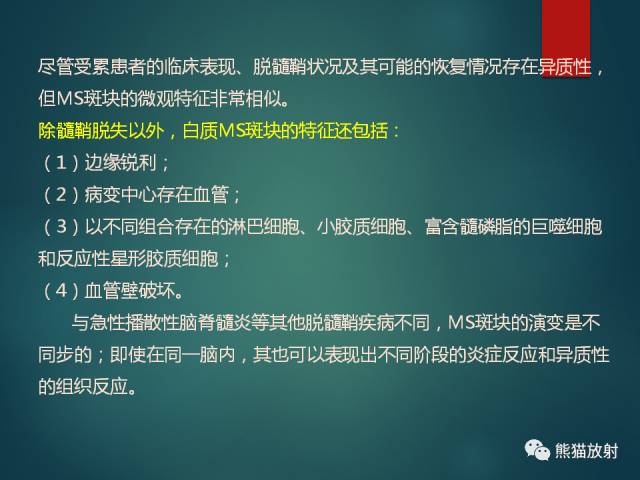
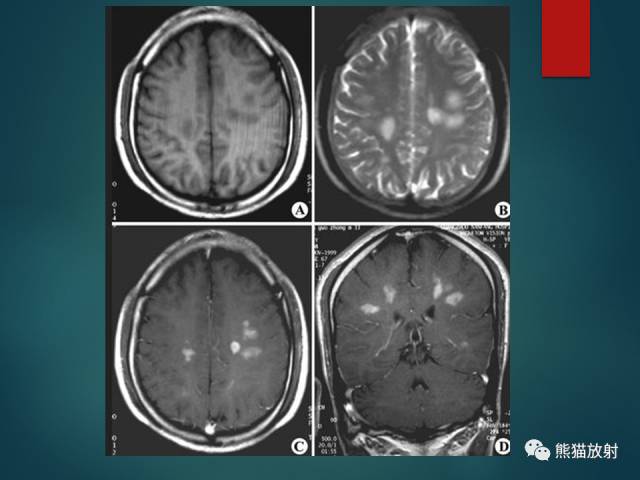
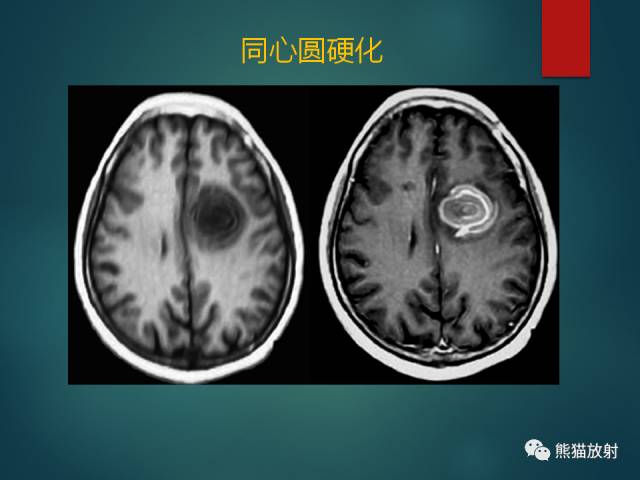
多发性硬化(MS):中青年女性;症状发作与缓解交替出现;直角脱髓鞘征;不同时期脱髓鞘斑块表现不一,急性期有强化。
-
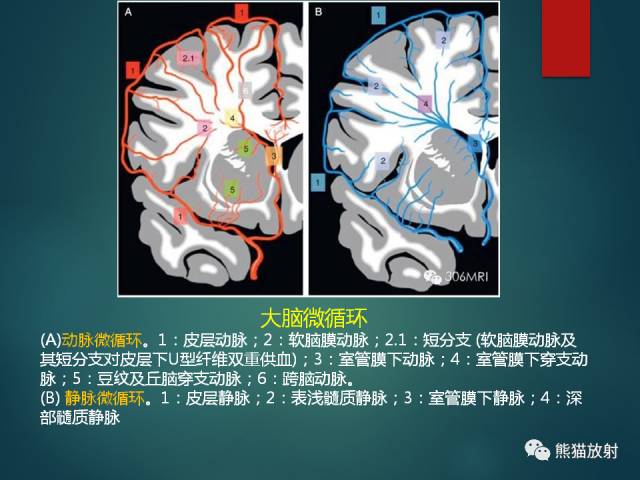
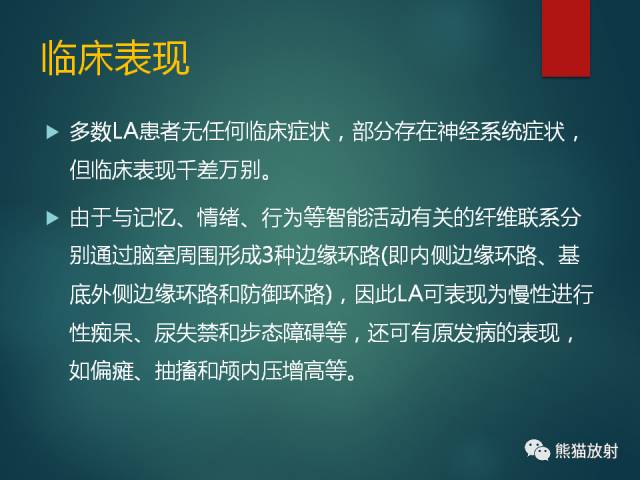
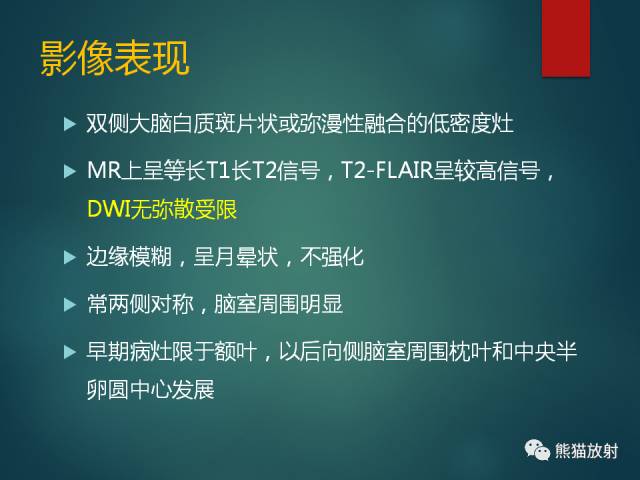
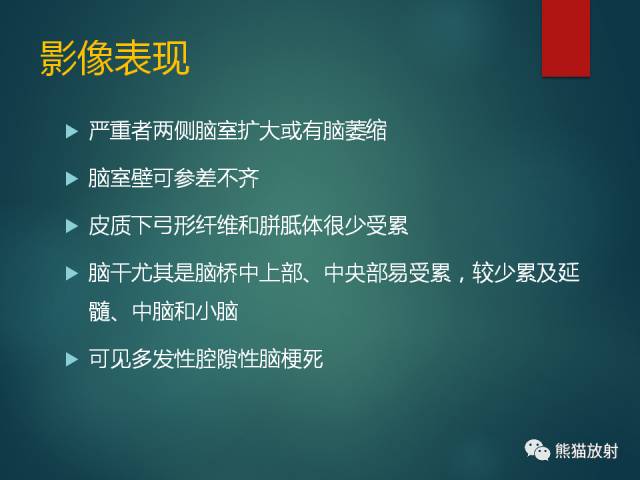
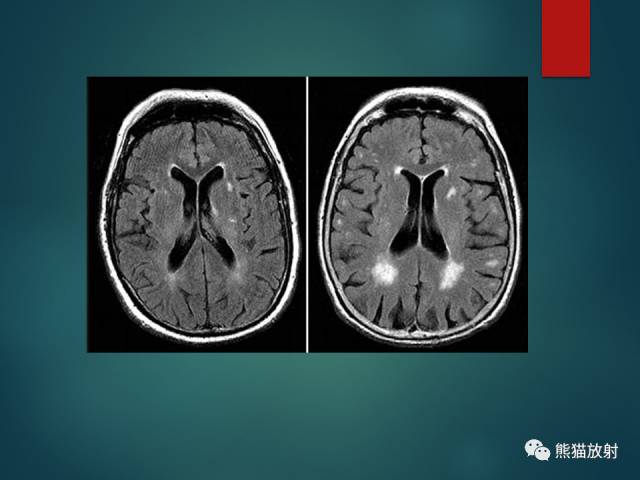
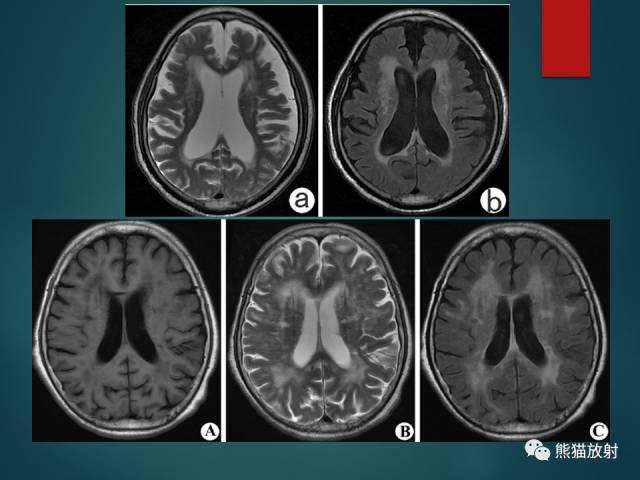
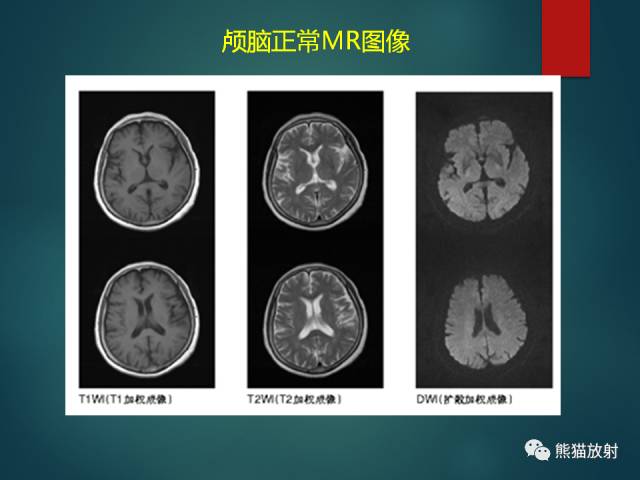
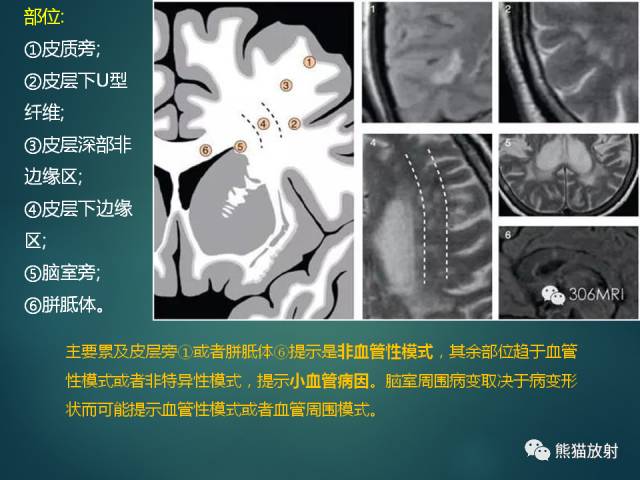
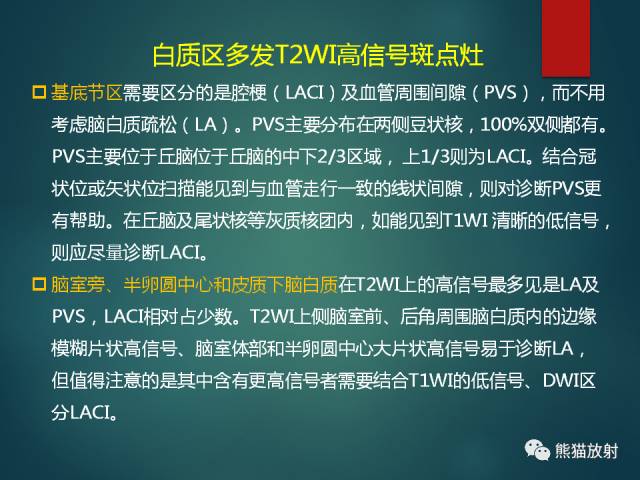
脑白质疏松(LA):小动脉病变导致的白质纤维脱髓鞘;T2-FLAIR呈较高信号,DWI无弥散受限;常两侧对称,脑室周围明显。
-
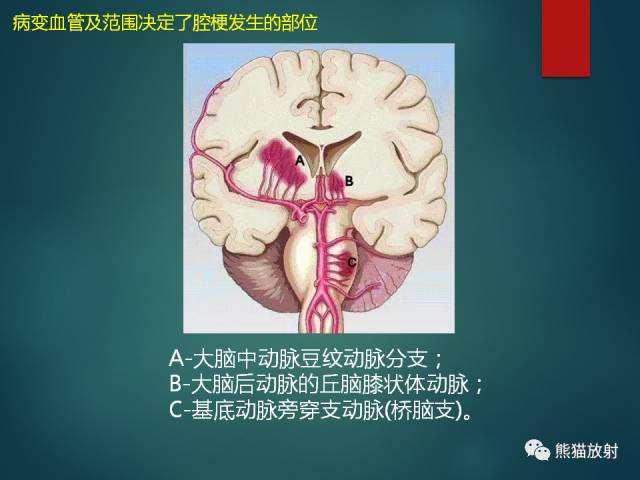
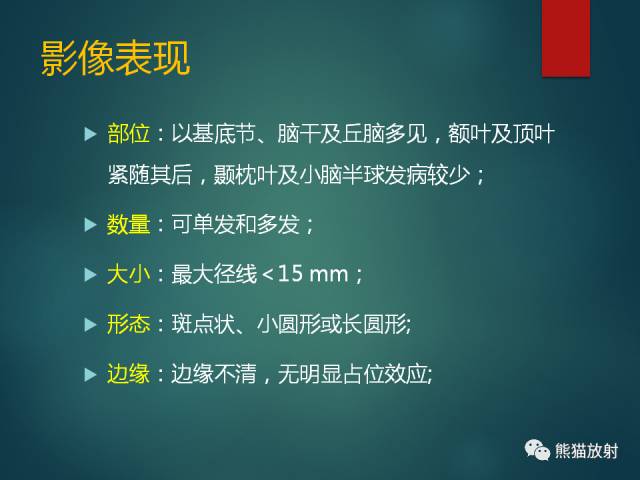
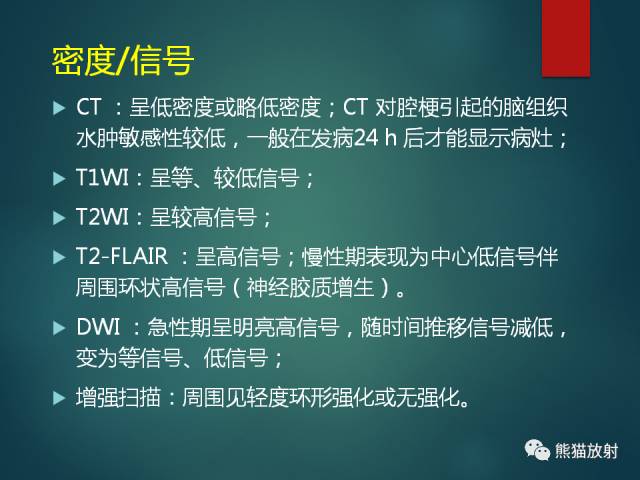
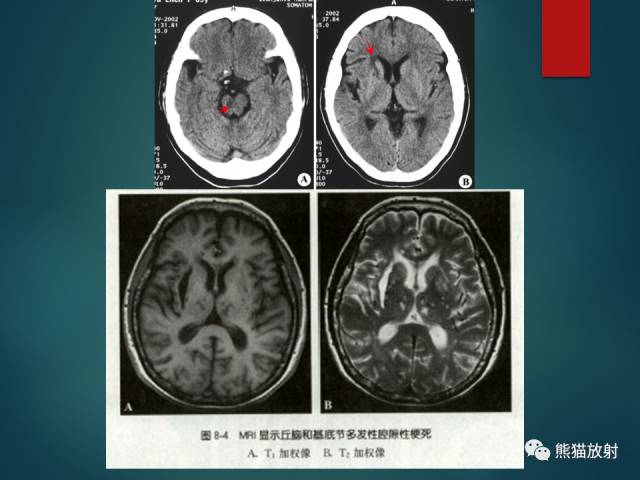
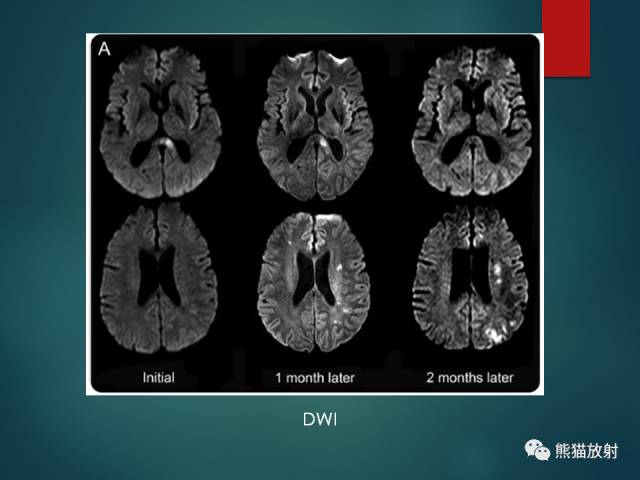
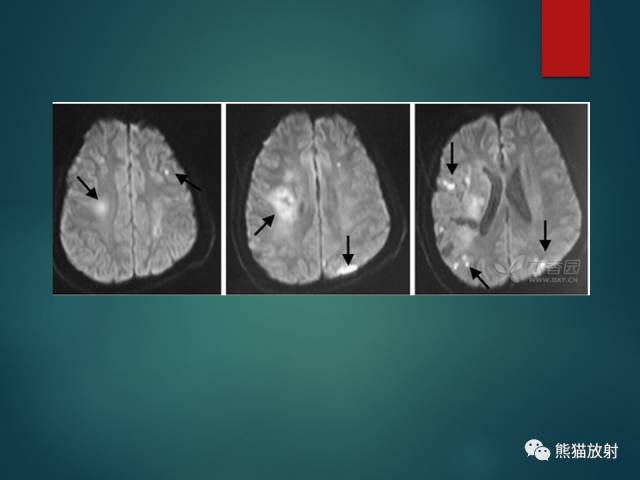
腔隙性脑梗死(LACI):颅内小动脉及穿支动脉狭窄或痉挛;T2-FLAIR呈高信号;DWI急性期弥散受限;基底节、脑干及丘脑多见。
-
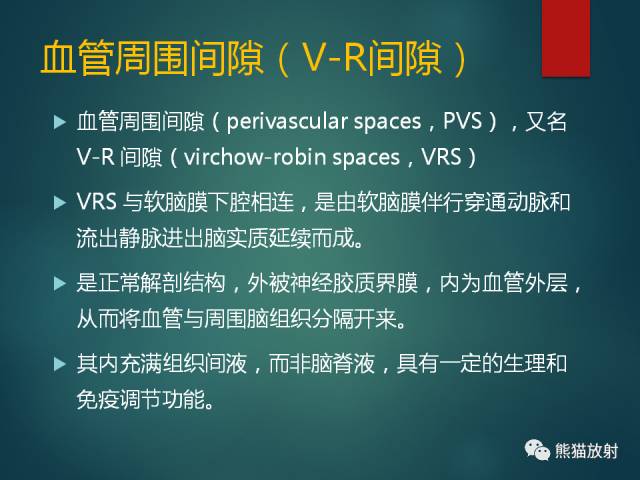
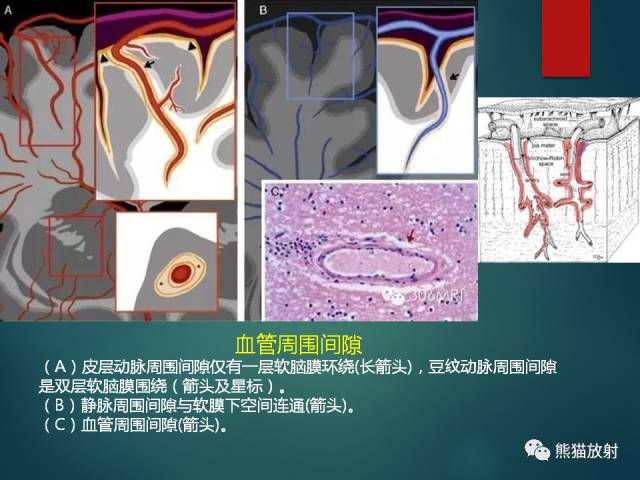
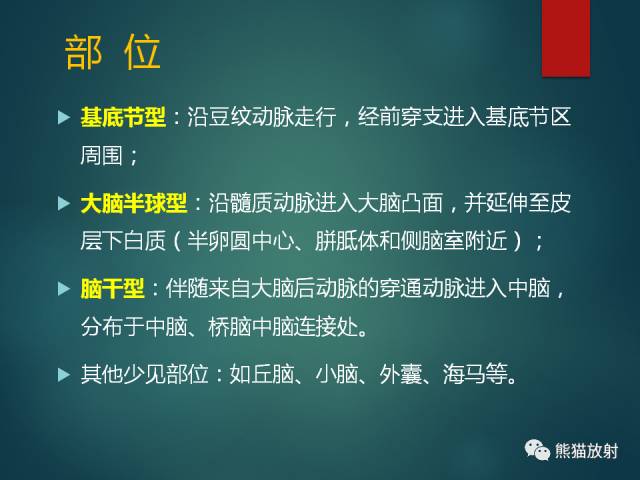
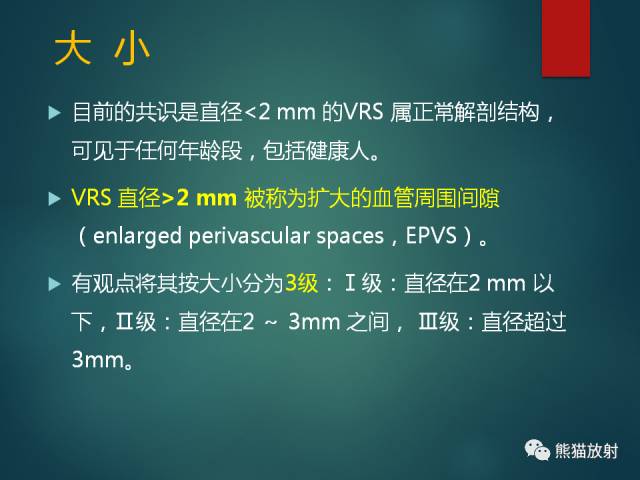
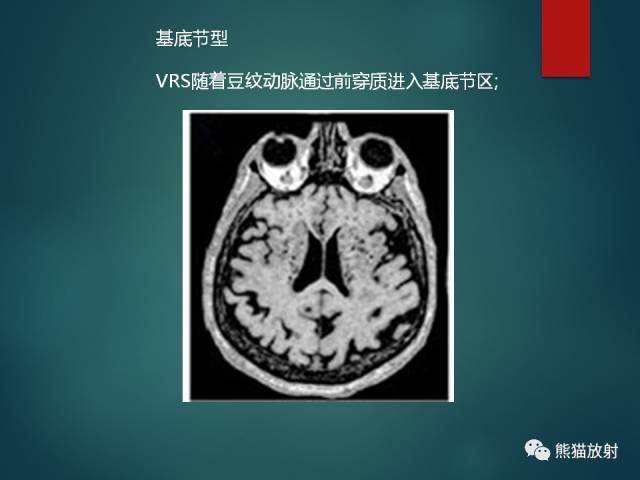
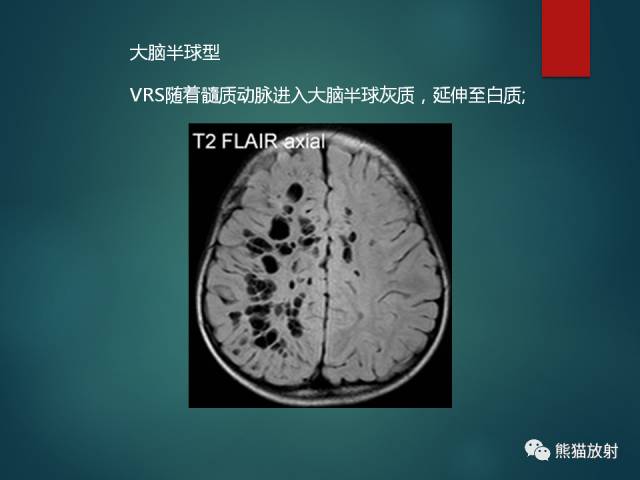
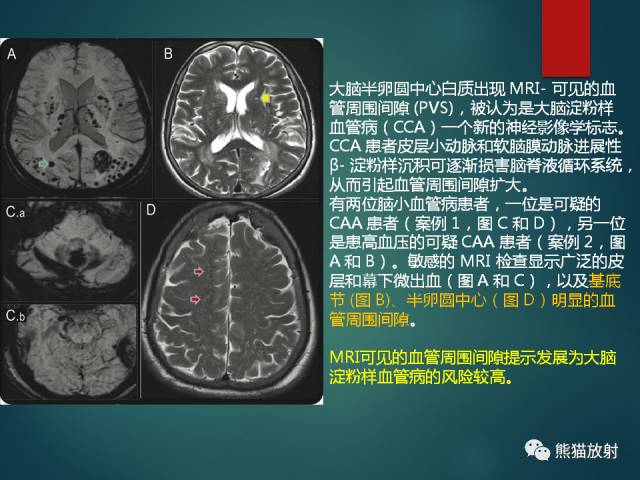
血管周围间隙(PVS):与软脑膜下腔相连;分为基底节型、大脑半球型及脑干型;与脑脊液信号相同。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#髓鞘#
34
#白质#
45
#高信号#
28
#变性#
37
#脱髓鞘#
29