CLIN CANCER RES:Binimetinib联合紫杉醇治疗铂类耐药卵巢癌
2018-11-20 MedSci MedSci原创
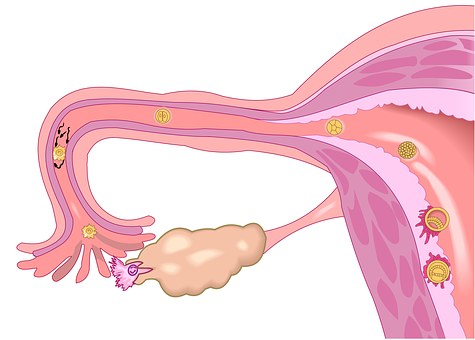
上皮性卵巢癌(EOC)是一种分子表型多样的肿瘤。MEK抑制靶向存在MAPK通路改变的肿瘤并增强紫杉醇诱导的细胞凋亡。CLIN CANCER RES近期发表了一篇文章,评估MEK抑制剂binimetinib联合紫杉醇治疗铂类耐药EOC患者的疗效。
上皮性卵巢癌(EOC)是一种分子表型多样的肿瘤。MEK抑制靶向存在MAPK通路改变的肿瘤并增强紫杉醇诱导的细胞凋亡。CLIN CANCER RES近期发表了一篇文章,评估MEK抑制剂binimetinib联合紫杉醇治疗铂类耐药EOC患者的疗效。
患者接受三种不同的静脉注射紫杉醇联合口服binimetinib给药方案。通过RECIST和CGIC CA-125反应标准评估结果。通过二代测序分析肿瘤样品。紫杉醇80mg / m 2静脉注射每周联合binimetinib30mg每天两次连续给药或45mg每天两次间间断性给药被确认是推荐II期试验剂量(RP2D)。3/4级不良反应发生率为65%。最佳总体反应率为18%,28例RECIST可测量疾病的患者中,1例完全缓解(CR)4,例部分缓解(PR),11,例患者达到稳定疾病(SD),临床获益率(CR + PR + SD)为57%。45mg每天两次的连续队列中RECIST和CA-125标准的缓解率在最高,45mg每天两次的间歇性队列中最低。4例存在MAPK通路改变的肿瘤患者均出现临床获益。
原始出处:
Zeynep Eroglu, Y. Ann Chen, et al. Combined BRAF and HSP90 Inhibition in Patients with Unresectable BRAFV600E-Mutant Melanoma. CLIN CANCER RES. November 2018 doi: 10.1158/1078-0432.CCR-18-0565
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#MET#
23
#铂类耐药#
46
#铂#
20
#binimetinib#
28
很好的学习机会
81
#铂类#
34