四川大学华西医院成功实施我国首例突破心脏"禁区"手术
2015-04-22 佚名 四川在线
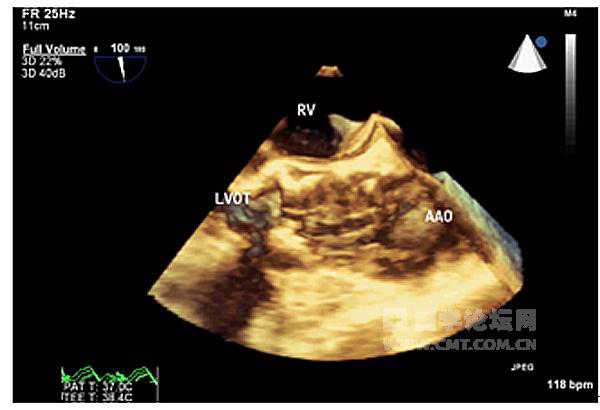
4月21日下午,川大华西医院宣布:在该院心脏大血管外科教授赁可带领下,医院的超声科、麻醉科、放射科及手术室的多学科协助,成功实施了我国首例突破心脏“禁区”的手术—经皮穿刺左心室入路的心脏手术,手术取得圆满成功,患者将于明日出院。43岁的宜宾人郑女士(化名)三年前因为风湿性心脏病,在当地医院接受了二尖瓣置换术。然而,手术第二年,曾经莫名的疲劳感又开始回到她身上,甚至还出现了呼吸困难、胸痛、尿少的情况
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#四川大学#
35
#西医院#
27
#四川大学华西医院#
33
#华西#
44
庆贺!
86