Oncologist:Toripalimab(特瑞普利单抗)联合紫杉醇+卡铂新辅助治疗可切除局部晚期食管鳞状细胞癌的疗效
2022-02-24 yd2015 MedSci原创
研究表明,Toripalimab(特瑞普利单抗)联合紫杉醇+卡铂可作为可切除局部晚期食管鳞状细胞癌的新辅助治疗方案。
免疫检查点抑制剂(ICIs)在晚期食管鳞状细胞癌(ESCC)治疗中是有效的;然而,它们在局部晚期可切除的食管鳞癌中的疗效和潜在的预测性生物标志物的数据有限。近期,四川肿瘤医院团队开展了相关研究,评估国产PD-1抑制剂Toripalimab(特瑞普利单抗)联合紫杉醇+卡铂新辅助治疗可切除局部晚期食管鳞状细胞癌的疗效。相关结果发表在Oncologist杂志上。
在这项研究中,纳入局部晚期可切除的ESCC患者。患者接受toripalimab(240mg/天,d1)+紫杉醇(135mg/m2,d1)和卡铂(AUC 5,d1)新辅助治疗,每三周一周期,共两周期,治疗4-6周后手术治疗。主要研究终点为安全性、可行性和主要病理反应(MPR)率;次要终点为病理完全缓解(pCR)率、无病生存期(DFS)和总生存期(OS)。
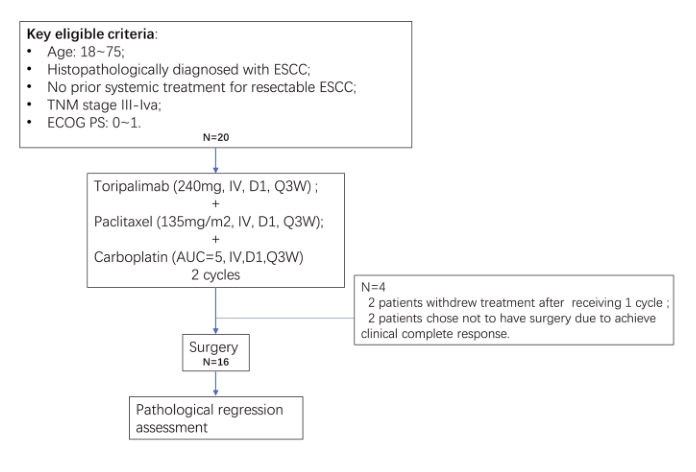
研究纳入20例可切除ESCC患者。其中,80%(16/20)患者为III期疾病,70%(14/20)患者为吸烟者或既往吸烟者,65%(13/20)患者有饮酒史。在新辅助治疗期间未观察到未报告的毒性。治疗相关的AEs发生在所有患者(20/20, 100%),最常见的AEs是恶心(15/20,75%)、贫血(14/20,70%)、脱发(9/20,45%)、白血球减少症(8/20,40%),和呕吐物(6/20,30)。4名患者(4/20,20.0%)经历了3级或更高的治疗相关的AEs,包括中性粒细胞减少(2/20,10.0%),白细胞减少(1/20,5.0%),疲劳(1/20,5.0%)。未发生治疗相关死亡。

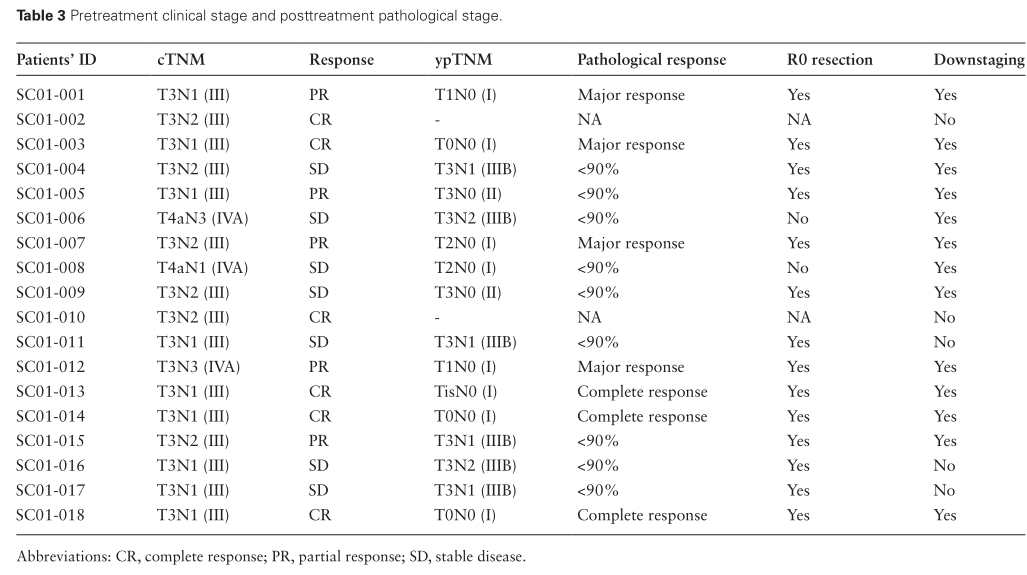
18例患者中,完全缓解6例(6/18,33.3%),部分缓解5例(5/18,27.8%),病情稳定7例(7/18,38.9%),无患者出现进展性疾病(PD)。13例患者(13/18,72.2%)出现病理降期。
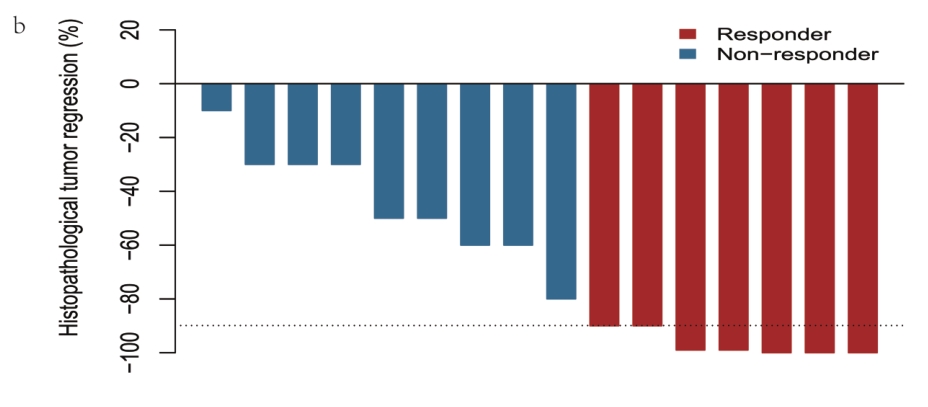
16例患者均行手术,无治疗相关手术延误,R0切除率为87.5%(14/16)。16例患者中MPR率为43.8% (7/16),pCR率为18.8%(3/16)。
在接受新辅助治疗出现应答的患者中,手术标本中CD8 + T细胞的丰度增加(P =0 .0093),伴有M2型肿瘤相关巨噬细胞比例减少(P =0.036)。新辅助治疗出现应答者与基线时CXCL5的基因表达水平较高(P = 0.03)、CCL19的基线水平较低(P =0 .017)和UMODL1的基线水平较低(P =0 .03)相关。
综上,研究表明,Toripalimab(特瑞普利单抗)联合紫杉醇+卡铂可作为可切除局部晚期食管鳞状细胞癌的新辅助治疗方案。
原始出处:
Wenwu He 1, Xuefeng Leng , Tianqin Mao, et al. Toripalimab Plus Paclitaxel and Carboplatin as Neoadjuvant Therapy in Locally Advanced Resectable Esophageal Squamous Cell Carcinoma. The Oncologist, 2022, 27, e18–e28. https://doi.org/10.1093/oncolo/oyab011.Advance access publication 28 January 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











上海哪家医院有这种治疗方法?食管癌
33
#细胞癌#
54
#Oncol#
40
#瑞普利单抗#
45
#局部晚期#
36
#新辅助#
40
#铂#
31
#mAb#
35
#食管鳞状细胞癌#
55
#卡铂#
67