胸痛但冠脉造影正常,应警惕这五种微循环功能异常
2017-03-20 岱西 中国循环杂志
许多胸痛患者行冠状动脉造影时并不显示心外膜冠脉阻塞病变,这可能与冠状动脉微循环功能障碍相关。那么如何改善冠状动脉微循环功能障碍?
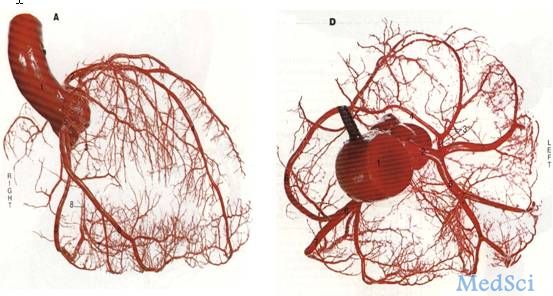
许多胸痛患者行冠状动脉造影时并不显示心外膜冠脉阻塞病变,这可能与冠状动脉微循环功能障碍相关。那么如何改善冠状动脉微循环功能障碍?
河北省人民医院李树仁、马玉龙在本刊就此进行了阐述,并指出,临床上应对胸痛患者进行冠状动脉微循环功能评估,尤其对于行冠状动脉造影显示正常或接近正常的患者。
冠状动脉微循环功能障碍主要分五型
这五型包括:(1)原发性无结构性心脏病存在;(2)存在心肌病变(左心室肥厚、肥厚型心肌病、扩张型心肌病及心肌淀粉样变);(3)合并有阻塞性冠心病;(4)冠状动脉介入治疗后;(5)心脏移植术后。
其中,微血管阻力指数(IMR)作为一种简单、强大及可重现的方法可准确评估冠状动脉微循环状态。
冠状动脉微循环功能障碍的的治疗措施
阻塞性冠心病:国外学者提出了几种治疗方案包括硝普钠、腺苷、维拉帕米及其他血管扩张剂治疗冠状动脉血流量不足。
此外,还有数项研究显示,急诊PCI术后应用尼可地尔,可更有效降低患者微循环功能障碍发生率。
还有研究显示,广泛血栓形成的患者可从辅助治疗策略中受益,如进一步的血栓抽吸或应用血小板糖蛋白Ⅱb/ Ⅲa(GP Ⅱb/ Ⅲa)拮抗剂。
肥厚型心肌病:无水酒精室间隔消融术可增加冠状动脉血流储备及心内膜向心外膜心肌血流量,而维拉帕米、丙吡胺及ACEI未能改善心肌灌注。
扩张型心肌病:β受体阻滞剂、别嘌呤醇有助于改善冠状动脉微血管功能障碍。
急性心肌炎:迄今为止没有更好的措施可改善这些患者微血管功能障碍。
主动脉瓣狭窄:β受体阻滞剂可延迟心肌缺血及心绞痛的发作。如果有禁忌或不能耐受β受体阻滞剂,可选用伊伐布雷定。然而,这些药物改善冠状动脉微血管灌注、心绞痛发作的临床效果缺乏大规模试验,因此应进行前瞻性随机试验研究。
原始出处:
马玉龙, 李树仁. 冠状动脉微循环功能障碍的研究进展. 中国循环杂志, 2016, 31: 619-621.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#功能异常#
40
#微循环#
27
#冠脉造影#
40
#造影#
29