Spine J:瘫痪患者行手术,有助于驾车安全
2015-05-13 MedSci MedSci原创
背景:已有多项研究报道了数种手术对患者术后驾驶反应时间(DRT/driving reaction time)的影响。然而作为脊柱疾病中最常见的一种:腰椎间盘突出症,其手术对驾驶反应时间的影响却从未被报道过。 目的:分析腰椎间盘突出症引起的左侧或右侧瘫痪患者术前及术后驾驶反应时间的差距。 方法:本实验为前瞻性临床对照试验,纳入者均为即将进行腰椎间盘手术的患者。本实验所考察的指

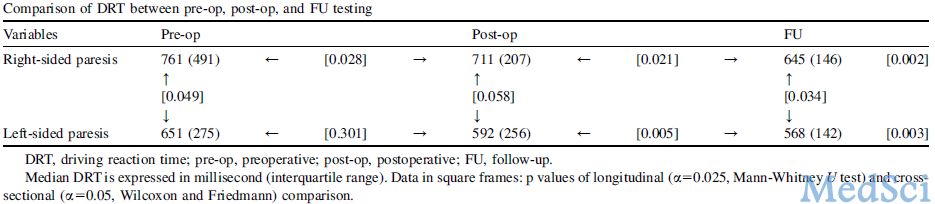
方法:本实验为前瞻性临床对照试验,纳入者均为即将进行腰椎间盘手术的患者。本实验所考察的指标为腰椎间盘突出症引起的瘫痪和腰椎间盘手术分别对驾驶反应时间造成的影响。连续42位患者(平均50.3岁)在术前1天,出院前及术后5周接受了测试。
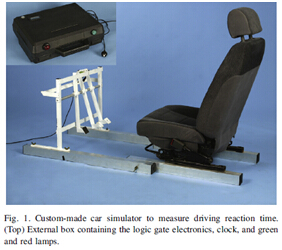
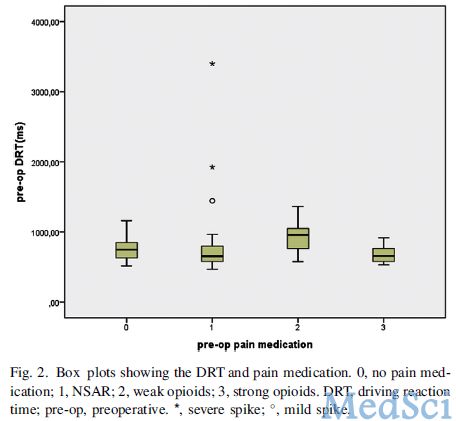
除了驾驶反应时间之外,记录指标还包括用视觉模拟评分法(VAS/visual analogue scale)记录的腰腿痛的程度,疼痛的治疗方法以及患者驾驶的频率。驾驶反应时间由自制的汽车模拟器测试,当受试者踩下油门时,测试绿灯亮。然后观察者(在受试者看不见的地方)打开红灯,此时要求受试者尽可能快的踩下刹车,这之间的时间间隔即为驾驶反应时间。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
32
很用心意啊
68
#瘫痪#
31
看看
113