PET诊断早期肺癌N1淋巴结转移准确性欠佳
2015-01-15 baofeichao 丁香园
近年来,早期肺癌的非外科性的局部治疗,如体外定向放射治疗,消融治疗等局部治疗,其应用逐渐增多,虽然肺癌局部治疗患者往往死于远处转移,但也有一部分患者是因为局部淋巴结控制不佳所致。因此局部治疗前需明确患者是否存在N1淋巴结的转移,而PET是判断淋巴结是否存在转移较好的非侵袭性诊断方法,但其用于诊断肺癌N1淋巴结转移评估的报道目前较少。 近日,来自MD-Anderson癌症中心的Swishe
近年来,早期肺癌的非外科性的局部治疗,如体外定向放射治疗,消融治疗等局部治疗,其应用逐渐增多,虽然肺癌局部治疗患者往往死于远处转移,但也有一部分患者是因为局部淋巴结控制不佳所致。因此局部治疗前需明确患者是否存在N1淋巴结的转移,而PET是判断淋巴结是否存在转移较好的非侵袭性诊断方法,但其用于诊断肺癌N1淋巴结转移评估的报道目前较少。
近日,来自MD-Anderson癌症中心的Swisher博士等评估了PET在诊断肺癌N1淋巴结转移中的价值,同时比较了经PET评估的N1阳性和阴性患者的长期生存,该研究结果发表在最先的Annals of Thoracic Surgery。
该研究为回顾性研究,初步纳入877例术前行PET检查的cN0患者,术后病理提示93例(11%)患者为pN1,86例(10%)患者为pN2。PET诊断N1淋巴结是否存在转移的敏感性为22%,特异性为93%,阴性预测值为79%,阳性预测值为50%。
该研究进一步纳入术前行PET检查,术后病理例证实为T1-2N1M0(II期)的肺癌患者104例,其中IIA期(T1aN1,T1bN1或T2aN1)87例,IIB期(T2bN1)17例。

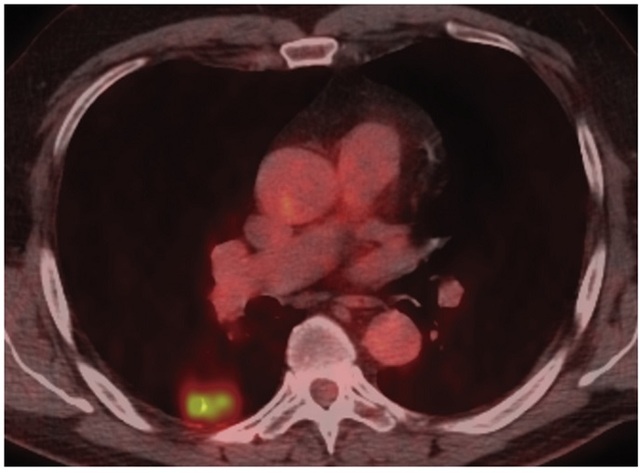
图1. PET提示周围型肺癌SUV值升高(SUVmax=6),而N1淋巴结SUV值均为见明显升高,术后病理证实患者为N1阳性。
结果发现104例pN1患者中,术前PET检查提示为N1阳性的患者为25例(24%,图1),其余79例术前PET检查N1均为阴性,前者3年生存率为63%,中位生存期为64.7月,而后者3年生存率为66%,中位生存期为54月,两组患者间生存无显著性差异(图2)。

图2. 术前PET提示N1阳性的患者与N1阴性患者的生存曲线.
(虚线所示为PET提示N1阳性患者,实线则为PET提示N1阴性患者)
综上研究结果,Swisher博士等认为PET诊断肺癌N1淋巴结是否存在转移敏感性欠佳,不能单一的将PET用于评估非外科性局部治疗的肺癌患者是否存在N1淋巴结转移。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#准确性#
0
#PE#
37
#早期肺癌#
36
#淋巴结#
21
#淋巴结转移#
28
#PET#
33
那么有没有更好的方法判断呢?
43