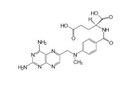
LANCET:甲氨蝶呤能否增加关节内皮质类固醇对幼年关节炎的疗效?
2017-02-07 MedSci MedSci原创
\目前,很少有基于证据的信息可用于指导治疗低聚幼年特发性关节炎。近期,一项发表在权威杂志LANCET上的文章研究了口服甲氨蝶呤能否增加关节内皮质类固醇的疗效。这是一项在意大利十家医院进行的前瞻性、开放性、随机试验。将18岁以下的患病儿童随机分配(1:1)分为单独关节内予以皮质类固醇或与口服甲氨蝶呤组合(15mg / m 2;最大20mg)两组。使用的皮质类固醇是曲安奈德(肩、肘、腕、膝和胫骨关节)
\目前,很少有基于证据的信息可用于指导治疗低聚幼年特发性关节炎。近期,一项发表在权威杂志LANCET上的文章研究了口服甲氨蝶呤能否增加关节内皮质类固醇的疗效。
这是一项在意大利十家医院进行的前瞻性、开放性、随机试验。将18岁以下的患病儿童随机分配(1:1)分为单独关节内予以皮质类固醇或与口服甲氨蝶呤组合(15mg / m 2;最大20mg)两组。使用的皮质类固醇是曲安奈德(肩、肘、腕、膝和胫骨关节)或醋酸甲泼尼龙(如距下和跗骨关节)。此项研究没有掩盖患者或研究者治疗分配的信息。研究的主要结果是意向治疗人群中在12个月时所有注射关节中关节炎缓解的患者比例。该试验在欧盟临床试验注册登记,EudraCT号2008-006741-70。
研究结果显示:2009年7月7日至2013年3月31日,共筛选226名参与者,随机分配102名患者进行单独的关节内皮质类固醇治疗;105名患者进行关节内皮质类固醇加甲氨蝶呤治疗。单独使用关节内皮质类固醇治疗组中有33例(32%)患者,关节内皮质类固醇和甲氨蝶呤联合治疗组有39例(37%)患者所有注射关节的关节炎得到缓解(p = 0.48)。接受甲氨蝶呤联合治疗组中有20名(17%)患者出现不良事件,其中有两名患者永久治疗停止(一名由于肝转氨酶增加,一名由于胃肠道不适)。没有患者发生严重不良事件。
此项研究得出结论:联合予以甲氨蝶呤没有增加关节内皮质类固醇治疗的有效性。需要进一步的研究来确定最佳治疗策略。
原始出处:
Ravelli A, Davì S, Bracciolini G, et al. Intra-articular corticosteroids versus intra-articular corticosteroids plus methotrexate in oligoarticular juvenile idiopathic arthritis: a multicentre, prospective, randomised, open-label trial. Lancet. 2017 Feb 2. pii: S0140-6736(17)30065-X.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Lancet#
28
#关节炎#
29
#类固醇#
28
学习了,谢谢!
69
学习了,非常好
74
长见识了
67