2018CCCP&SCC:李妍教授畅谈OCT对复杂高危患者的指导价值
2018-04-08 国际循环编辑部 国际循环
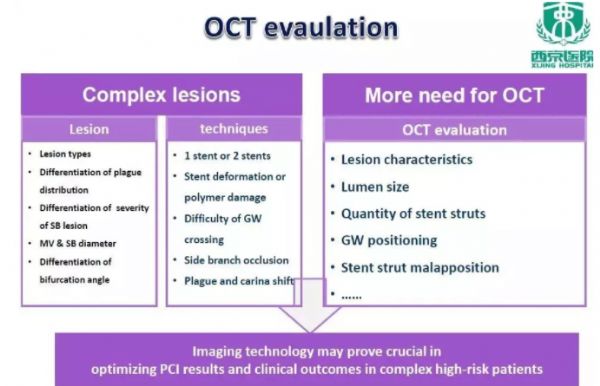
复杂高危且有介入治疗指征的患者(CHIP)的经皮冠状动脉介入(PCI)治疗一直是介入治疗领域关注的焦点和难点。光学相干断层扫描(OCT)等影像学技术为上述患者的治疗提供了重要指导价值。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#SCC#
36
#高危患者#
39
#OCT#
35
好文章学习了
86
不错很喜欢很实用.值得推荐
91