盘点:心血管疾病介入治疗指南与共识(上)
2016-08-26 MedSci MedSci原创
一、2016 经皮冠状动脉介入治疗术后运动康复专家共识经皮冠状动脉介入治疗( percutaneous coronaryintervention,PCI) 已成为冠心病患者最重要的血运重建手段。 然而,仅通过 PCI 术和药物治疗并不能持续有效改善患者的预后。PCI 术既不能逆转或减缓冠状动脉粥样硬化的生物学进程,也不能消除冠心病危险因素。多数患者存在的术后运动耐量下降及焦虑抑郁等精神问题,不仅严
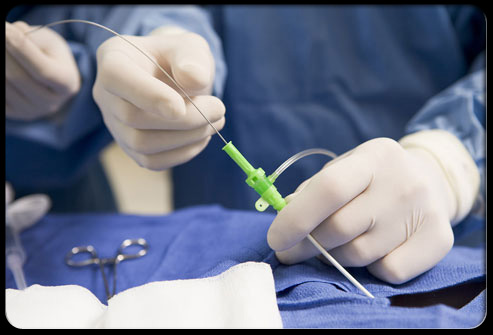
冠状动脉粥样硬化性心脏病(简称冠心病)是当今世界威胁人类健康最重要的心血管疾病之一,其主要病理生理机制是冠状动脉粥样硬化狭窄或阻塞所致的心肌缺血坏死。心肌血运重建治疗是指以冠状动脉介入或外科手术方法解除冠状动脉狭窄、重建血管,恢复心肌灌注,目前最主要的方法包括经皮冠状动脉介入治疗(PCI)、冠状动脉旁路移植术(CABG)和二者结合的杂交手术治疗。梅斯小编对最近几年发布的心血管疾病介入治疗指南与共识进行了整理,与大家分享。
经皮冠状动脉介入治疗( percutaneous coronaryintervention,PCI) 已成为冠心病患者最重要的血运重建手段。 然而,仅通过 PCI 术和药物治疗并不能持续有效改善患者的预后。PCI 术既不能逆转或减缓冠状动脉粥样硬化的生物学进程,也不能消除冠心病危险因素。多数患者存在的术后运动耐量下降及焦虑抑郁等精神问题,不仅严重影响生活质量,也给家庭及国家带来巨大经济负担和劳动力损失。因此,运动康复及二级预防在发达国家蓬勃发展,并成为 PCI 术后治疗的重要辅助手段。(文章详见——2016 经皮冠状动脉介入治疗术后运动康复专家共识)

二、2015 ACC/AHA/SCAI指南:直接经皮冠状动脉介入治疗ST段抬高型心肌梗死
2015年10月,美国ACC/AHA/SCAI三大学会联合对STEMI患者直接经皮冠脉介入治疗(PCI)指南进行了更新,此次更新的证据是主要来自多项重要试验。(文章详见——2015 ACC/AHA/SCAI指南:直接经皮冠状动脉介入治疗ST段抬高型心肌梗死)
三、2014 经皮冠状动脉介入治疗(PCI)手术前后抑郁和(或)焦虑中医诊疗专家共识
中华中医药学会介入心脏病学专家委员会组织相关专家,以中医学基本证候和经验,制定PCI术后抑郁和(或)焦虑中医诊疗专家共识,以提高临床疗效,促进学术交流。(文章详见——2014 经皮冠状动脉介入治疗(PCI)手术前后抑郁和(或)焦虑中医诊疗专家共识)
四、2014 ESC/EHRA/EAPCI/ACCA联合共识:非瓣膜病房颤合并急性冠脉综合征和/或拟接受经皮冠脉或瓣膜介入术患者的抗凝治疗管理
2014年8月,欧洲心脏病学会(ESC,European Society of Cardiology)联合EHRA、EAPCI、ACCA共同发布本共识。(文章详见——2014 ESC/EHRA/EAPCI/ACCA联合共识:非瓣膜病房颤合并急性冠脉综合征和/或拟接受经皮冠脉或瓣膜介入术患者的抗凝治疗管理)
五、2014 经皮冠状动脉介入治疗(PCI)术后胸痛中医诊疗专家共识
经皮冠状动脉介入治疗(PCI)术后仍有不少患者发生胸痛,其发生率高达50%。PCI术后胸痛属于中医“胸痹心痛”范畴。为了提高中医临床诊疗PCI术后胸痛的水平,中华中医药学会介入心脏病学专家委员会组织相关专家,以传统中医学基本证候和相应方药为基本点,结合现代临床研究进展和专家临床经验,制订PCI术后胸痛中医诊疗专家共识,经中华中医药学会介入心脏病学专家委员会讨论通过。(文章详见——2014 经皮冠状动脉介入治疗(PCI)术后胸痛中医诊疗专家共识)
六、2014 SCAI/ACC/AHA 无现场外科手术支持的经皮冠状动脉介入(PCI)专家共识-更新版
2014年3月17日,美国SCAI/ACC/AHA三大学会在线发布了没有现场外科手术支持的经皮冠状动脉介入(PCI)专家共识的更新文件。该共识文件(指南)对过去十年中PCI的进展进行了回顾,提出了多项新的建议,是对2007年SCAI文件的更新,而后者是该领域的第一个共识文件。该文件同时发表于《Catheterization & Cardiovascular Interventions》、《the Journal of the American College of Cardiology》和《Circulation》。(文章详见——2014 SCAI/ACC/AHA 无现场外科手术支持的经皮冠状动脉介入(PCI)专家共识-更新版)
七、2013 ACC/AHA/SCAI/AMA 成人经皮冠状动脉介入术(PCI)执行和质量评估报告
2013年12月19日,美国心脏病学会(ACC)和美国心脏协会(AHA)联合心血管造影和介入学会(SCAI)、美国医学会(AMA)、国家质量保证委员会(NCQA)等多个组织发布了最新的《成人经皮冠状动脉介入术(PCI)执行和质量评估报告》。报告全文于2013年12月19日在线发表于《J Am Coll Cardiol 》和《Circulation》杂志。ACC/AHA绩效评估工作组指出,这些新的措施将获取质量相关的重要方面,包括PCI的及时性、安全性、效率和效益,以及其他方面,同时试图减少医生的报告负担。(文章详见——2013 ACC/AHA/SCAI/AMA 成人经皮冠状动脉介入术(PCI)执行和质量评估报告)
八、2013 SCAI 经桡动脉径介入治疗专家共识
在美国的心脏导管室采用经桡动脉径路作为介入途径的手术方法日益增多,因此美国的心血管造影和介入协会公布了一项专家共识以对此技术进行了规范。(文章详见——2013 SCAI 经桡动脉径介入治疗专家共识)
九、2013 CCS立场声明:来自心脏成像和介入手术的辐射曝露
2013年9月10日,加拿大心血管学会(CCS)发布了关于来自心脏成像和介入手术的辐射曝露的立场声明。(文章详见——2013 CCS立场声明:来自心脏成像和介入手术的辐射曝露)
本文系梅斯医学(MedSci)原创编译整理,转载需授权!更多资讯,请下载"辣眼睛的医学科研神器之梅斯医学APP”!扫一下二维码即可:

版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#治疗指南#
30
文章很好值得关注
69
学习了啊
68
谢谢分享,学习了
62
#血管疾病#
41
值得学习
66
阅读了。
0