Am J Hematol:癌症住院患者静脉血栓栓塞风险 KS预测工具是否有效
2017-06-16 梁舒瑶 环球医学资讯
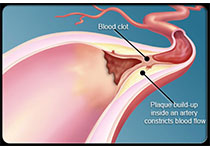
静脉血栓栓塞(VTE)是一种需要住院患者重点预防的疾病;癌症的风险多样,而预防是一致的。既往证实的工具(Khorana评分,[KS])由5个容易获得的变量组成,可以确定门诊癌症患者的VTE风险,但该工具尚未在住院患者中研究过。2017年6月,发表在《Am J Hematol》的一项回顾性队列研究评价了KS预测癌症住院患者VTE风险的有效性。
Patell, R., et al.Predicting risk of venous thromboembolism in hospitalized cancer patients: Utility of a risk assessment tool. Am J Hematol. 2017 Jun;92(6):501-507. doi: 10.1002/ajh.24700. Epub 2017 May 2.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#静脉#
36
#静脉血栓栓塞风险#
47
#静脉血#
0
文章很好,值得拜读
65
学习了谢谢分享!!
49
文章很好,值得拜读
43
#EMA#
24
学习了,谢谢分享
46
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了,点个赞吧!
0
学习了,谢谢分享
24