BMJ:新生儿首次胎粪记录的重要性-案例报道
2017-03-18 xing.T MedSci原创
该婴儿被给予静脉补液,并进行钡剂灌肠、直肠冲洗。吸取直肠活检证实为赫希施普龙氏病的诊断。该患者接受了手术治疗,术后康复平稳。4年后随访,该患者恢复很好,将继续跟进随访。家长能够意识到患儿症状与赫希施普龙氏病相关的小肠结肠炎风险。
患者为足月出生的2天大男婴,因进展性腹胀以及出生头24小时内没有排便而转诊至新生儿手术中心。体检男婴体重 2.9公斤和肛门位置正常。进行心血管、呼吸和其他系统检查以及一个简单的发育评估,结果均正常。腹部扩张,但无腹膜炎特点。婴儿血流动力学稳定。
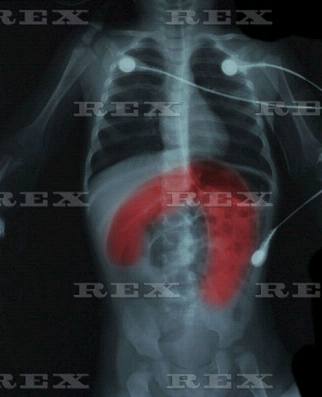
血化验结果均正常,包括全血细胞计数、尿素和电解质类、C-反应蛋白、凝血功能。腹部的X线片呈均匀分布整体扩张的肠管,直肠没有气体。一种水溶性造影剂灌肠显示造影剂可以通过远端结肠到扩张的近端正常结肠。在病房吸取直肠活检进行组织病理学评价。
问题
1、诊断是什么?鉴别诊断有哪些?
赫希施普龙氏病(先天性巨结肠症)(图1)。需要进行鉴别诊断的疾病包括:肛门直肠畸形、胎粪阻塞综合征、小左结肠综合征、肠闭锁、胎粪性肠梗阻和回肠闭锁。
2、该病如何治疗?
病人必须先给予静脉输液,其次是进行直肠冲洗减压。如果存在赫希施普龙氏病相关的小肠结肠炎给予广谱抗生素静脉输液治疗。然后需要接受手术进行根治性治疗。
3、该病的长期并发症有哪些?
术后最常见的长期并发症包括便秘、大便失禁和肠炎。肠炎可发生手术矫正前后,并且可危及生命。
患者预后
该婴儿被给予静脉补液,并进行钡剂灌肠、直肠冲洗。吸取直肠活检证实为赫希施普龙氏病的诊断。该患者接受了手术治疗,术后康复平稳。4年后随访,该患者恢复很好,将继续跟进随访。家长能够意识到患儿症状与赫希施普龙氏病相关的小肠结肠炎风险。
原始出处:
Daniel W Scholfield.et al. The importance of recording first passage of meconium in neonates. BMJ2017;356:j711 doi: 10.1136/bmj.j711
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#重要性#
36
#BMJ#
32
学习了
64
学习了
67
学习了,谢谢!
72
标题跟内容似乎不符啊
55
能够意识到患儿症状与赫希施普龙氏病相关的小肠结肠炎风险。
71
文章不错,值得分享
25