JCO:不幸中的万幸 —— ALK阳性脑转移NSCLC患者耐药后的新选择:Brigatinib
2018-05-28 慧语 肿瘤资讯
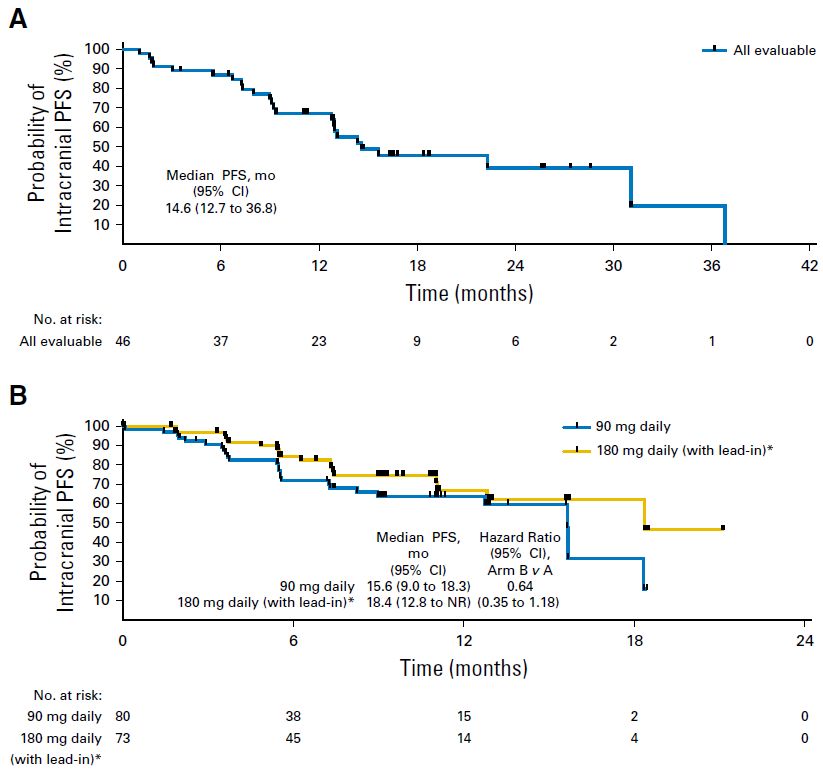
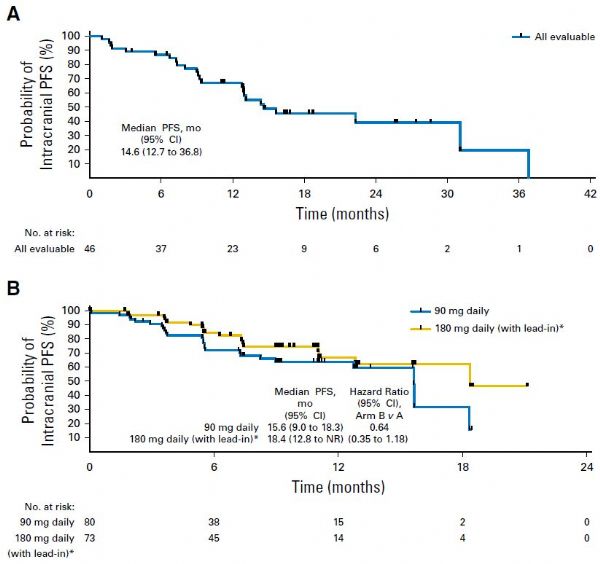
美国FDA于2011年批准克唑替尼治疗具有ALK基因重组的非小细胞肺癌(ALK阳性NSCLC)患者,但这些患者最终都会进展为耐药。并且而由于克唑替尼无法有效穿越血脑屏障,导致CNS是接受克唑替尼治疗后主要的转移部位之一。那么对于克唑替尼治疗失败且伴有脑转移的患者,我们束手无策了吗?别急,新一代ALK-TKI抑制剂Brigatinib来了!

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#ALK阳性#
26
#JCO#
40
#Brigatinib#
51
#SCLC患者#
26
学习了长知识
65
学习了长知识
1
学习了长知识
69
学习了长知识
64
学习了长知识
70
学习了长知识
28