病例回顾
患者女性,68岁。
主诉:因“脑外伤3个月余,呛咳6天”于2016年6月6日入院。
病史:患者3个月前因车祸入住外院行开颅血肿清除术,术后入住ICU,于2016年3月19日行气管切开术。2个月余后患者出现呛咳症状,胃镜检查提示距离门齿18cm可见食管瘘。后转至我院胸外科就诊。
查体:神志清楚,精神欠佳,颈部气管切开置管,双肺呼吸音略粗,可闻及少许湿啰音。
辅助检查:
实验室检查:白细胞计数9.5×109/L,血红蛋白11.6g/dL,血小板计数228×109/L,中性粒细胞百分数77.7%,超敏C反应蛋白43.7mg/L。
纤维气管镜(2016年6月7日):气管中段膜部距声门7cm左右见一瘘口,符合气管食管漏(TEF)诊断(图1)。

图1 纤维气管镜见气管漏口
治疗及复查结果:
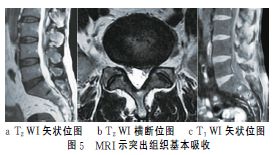
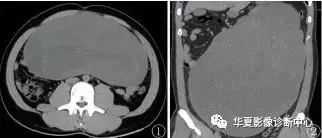
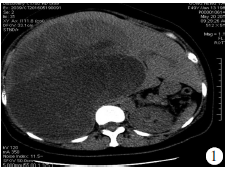
患者转呼吸内科拟行气管支架治疗,但是考虑到瘘口较大,位置不佳,无法行气管支架植入,遂选择行胃镜下经食管治疗。2016年6月23日床边胃镜检查见:距门齿20cm处可见一直径约4cm的瘘口,表面尚光滑,无明显分泌物,予一枚内镜金属夹系統(OTSC)及多枚钛夹补充夹闭瘘口,再经胃镜腔道置入鼻空肠营养管至十二指肠降部远端。术后禁食,肠内营养支持治疗。2016年7月1日复查颈部CT见:TEF术后,术区局部可见高密度影,符合TEF 治疗后改变。2016年7月11日纤维气管镜见(图2):气管中段膜部距声门7cm左右见一片六角形增生黏膜,与周围组织紧密粘合。因TEF形成时气管软骨环已破坏,术后增生黏膜非正常气管黏膜,考虑为纵隔软组织增生填塞了瘘口,至此患者的气道黏膜缺损已基本闭合。
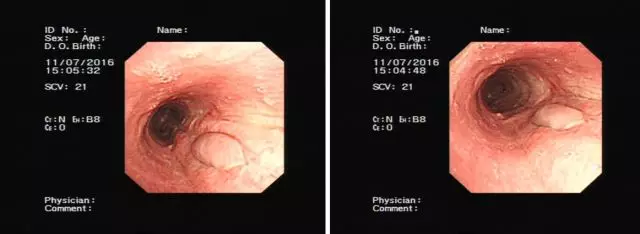
图2 纤维气管镜见术后食管黏膜增生
讨论
TEF临床上主要表现为反复肺部感染,进食呛咳,阵发性咳嗽,咯血等。根据病因可有良性和恶性之分。据文献 [1]报道其中47%良性TEF是由机械通气导致的,外伤后TEF形成占17%,恶性TEF中食管肿瘤占了75%。
TEF的内镜下支架植入术
既往TEF的治疗多采取外科手术治疗,但是外科手术创伤大,并发症多,死亡率也很高。近年来,随着内镜技术的发展,TEF可运用内镜治疗。内镜下气管支架植入封闭瘘口的同时可以改善气管狭窄,但是植入后不利于气管分泌物排出。对于高位的瘘口,食管支架往往是无法放置的。同时食管支架很容易移位,甚至可能移位至气管内造成气管梗阻,食管气管双支架植入适用于合并气管狭窄的恶性食管瘘的患者[2],但是其导致出血穿孔等并发症的可能性大大提高,另外术后吞咽困难伴胸痛等并发症也较常见。
对于恶性肿瘤导致的TEF患者,支架技术一定程度上可以改善预后,延长患者的生存期,但是对于良性病变导致的TEF,支架植入后常有胸部不适,对局部的压迫可能导致缺血坏死,造成瘘口增大,迁延不愈。并且良性病变愈合后支架取出时可能造成撕裂,使瘘口再次增大。综上,支架适用于瘘口小,生存期短的肿瘤性瘘口形成的患者,而对于高位瘘,瘘口较大以及良性病变导致的TEF是不适合放置支架的。
TEF的内镜下金属夹治疗
OTSC应用于消化道瘘的指征包括:
①7天以内的早期瘘口;
②消化道瘘口直径为1~3cm,
③瘘口周围少纤维化[3]。
对于慢性瘘道,周围组织已纤维化,直径>3cm,内镜下OTSC夹闭的成功率显著降低。Noriko报道了23例运用OTSC治疗ESD术后消化道穿孔的病例,其中9例病灶直径<2cm的患者均获得成功(成功率100%),8例直径2~3cm中2例治疗失败(成功率75%),6例直径>3cm中2例治疗失败(成功率66%),文中提到对于>3cm的病灶很难成功闭合[4]。Hang Lak Lee等的多中心前瞻性试验中[5]纳入了19个因自发性食管破裂导致的消化道瘘,OTSC治疗后均成功闭合瘘口,其中有2例TEF,分别是食管癌及肺结核病导致的瘘口,瘘口直径分别为8mm和5mm,这2个瘘口在OTSC操作上均获得了技术上的成功,但是通过长期随访发现临床上均以失败告终。很多文献已提到瘘口或者穿孔周围纤维硬化都直接影响临床成功率。这2个瘘口从形成到开始使用OTSC治疗的时间间隔较久,分别为15d和30d,其失败原因应该是瘘口边缘已逐渐纤维化。
本病例瘘口直径约4cm,属于慢性瘘道,我们运用OTSC与钛夹相结合,经治疗后1周复查颈部CT提示OTSC在位,2周后复查气管镜提示瘘口基本闭合。该例操作获得最终的成功,为OTSC治疗TEF的有效性提供了依据,为临床上治疗TEF又提供了更加合适的选择方案。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#食管瘘#
0
#治疗选择#
24
#气管食管瘘#
43
#病例讨论#
41
学习了,谢谢分享
65
#食管#
28
好文献学习了
47