European Urology:北京基因组所开发泌尿生殖系统肿瘤诊断和预后的液体活检技术
2019-11-22 北京基因所 北京基因所
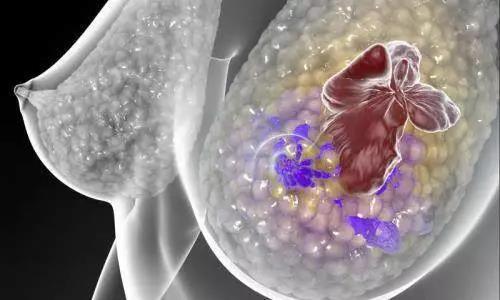
泌尿生殖系统(genitourinary, GU)肿瘤是指发生在泌尿生殖系统上的肿瘤,包括肾癌,尿路上皮癌,前列腺癌等。到 2020 年,全世界 GU 癌症的估计发病率将超过 200 万,死亡人数约 80 万人。目前对 GU 肿瘤的诊断和监测方法多为侵袭性和 / 或缺乏敏感性和特异性。液体活检技术凭借其无创或微创、实时监控等优势已然成为肿瘤研究领域的新兴技术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#生殖系#
38
#PE#
30
#生殖系统#
48
#液体活检技术#
39
#泌尿生殖系统肿瘤#
43
#活检#
33
#肿瘤诊断#
32