Sci Transl Med:液体活检再上一层楼!新技术助力乳腺癌预后监测,告别过度治疗!
2019-08-12 Ruthy 转化医学网
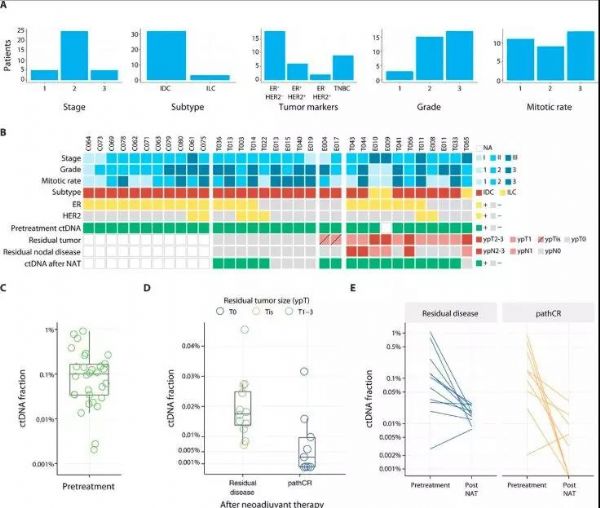
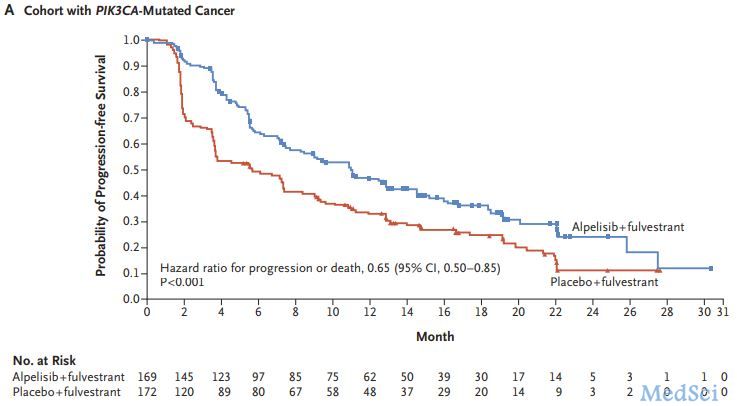
乳腺癌作为女性发病率首位的恶性肿瘤,在精准医学研究中占据着重要地位。以循ctDNA检测为代表的液体活检技术已成为乳腺癌精准诊治的重要工具,但该技术对微量ctDNA敏感性不高的问题仍然悬而未决。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#TRA#
22
#过度治疗#
48
#新技术#
21
#Transl#
33
#活检#
27
#Med#
31
学习了,学习了
58
好
67
好好好好好好
71