中国科学家发现提高T细胞抗肿瘤免疫功能新方法
2016-03-21 黄辛 科学网
中科院上海生科院生物化学与细胞生物学研究所分子生物学国家重点实验室/国家蛋白质科学中心(上海)许琛琦研究组和分子生物学国家重点实验室李伯良研究组在一项合作研究中发现“代谢检查点”可以调控T细胞的抗肿瘤活性,并鉴定了肿瘤免疫治疗的新靶点——胆固醇酯化酶ACAT1以及相应的小分子药物前体,为开发新的肿瘤免疫治疗方法奠定了基础。今天,题为“通过调节胆固醇代谢增强CD8+(加号是上标) T细胞的抗肿瘤
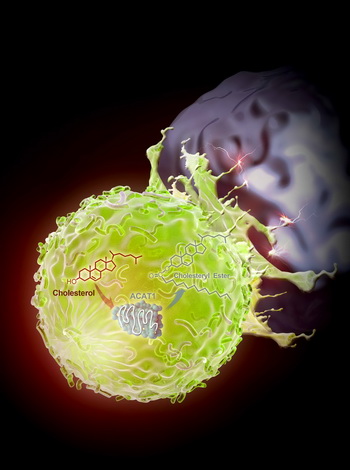
中科院上海生科院生物化学与细胞生物学研究所分子生物学国家重点实验室/国家蛋白质科学中心(上海)许琛琦研究组和分子生物学国家重点实验室李伯良研究组在一项合作研究中发现“代谢检查点”可以调控T细胞的抗肿瘤活性,并鉴定了肿瘤免疫治疗的新靶点——胆固醇酯化酶ACAT1以及相应的小分子药物前体,为开发新的肿瘤免疫治疗方法奠定了基础。今天,题为“通过调节胆固醇代谢增强CD8+(加号是上标) T细胞的抗肿瘤反应”的研究成果在线发表于国际顶尖学术期刊《自然》。
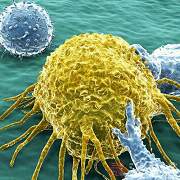
人体的免疫系统负责保卫机体健康,其中T细胞在肿瘤的监控和杀伤中起着至关重要的作用。然而肿瘤细胞能通过多种机制来抑制T细胞的抗肿瘤活性,从而逃避免疫系统的攻击。在临床上,可以通过提高T细胞的活性来治疗肿瘤。目前,基于T细胞的肿瘤免疫治疗已经取得巨大的成功,具有广泛的应用前景。但是现有的治疗方法只对部分病人有效,并有一定的副作用。因此科学家需要开发新的肿瘤免疫治疗方法来改善疗效并让更多的病人受益。
许琛琦研究团队和李伯良研究团队从全新角度去研究T细胞的抗肿瘤免疫功能。许琛琦研究员表示,通过调控T细胞的“代谢检查点”可改变其代谢状态,使其获得更强的抗肿瘤效应功能。研究人员发现T细胞代谢通路中的胆固醇酯化酶ACAT1是一个很好的调控靶点,抑制ACAT1的活性可以大大提高CD8+ T细胞(又名杀伤性T细胞)的抗肿瘤功能。因为ACAT1被抑制后,杀伤性T细胞膜上的游离胆固醇水平提高,从而让T细胞肿瘤抗原免疫应答变得更加高效。同时,研究人员还利用ACAT1的小分子抑制剂avasimibe在小鼠模型中治疗肿瘤,发现该抑制剂具有很好的抗肿瘤效应;并且avasimibe与现有的肿瘤免疫治疗临床药物anti-PD-1联用后效果更佳。
中国工程院院士王红阳点评该项研究成果:这是肿瘤免疫基础研究的一个重要突破,开辟肿瘤免疫治疗研究的一个全新领域,证明细胞代谢对肿瘤免疫应答起到了关键作用,同时发现ACAT1这一新的药物靶点,揭示ACAT1小分子抑制剂的应用前景,为肿瘤免疫治疗提供了新思路与新方法。
据介绍,这项研究得到了生化与细胞所刘小龙研究员,清华大学刘万里教授,武汉大学宋保亮教授,中山大学周鹏辉教授,美国德州大学安德森癌症中心孙少聪教授以及美国达特茅斯医学院Ta-Yuan Chang教授的大力帮助,并得到国家自然科学基金委、国家科技部、中国科学院先导专项及上海市科委的经费支持,同时得到国家蛋白质科学研究(上海)设施复合激光显微镜系统、生化与细胞所动物分析技术平台、细胞分析技术平台以及分子生物学技术平台的大力支持。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
相关资讯
中国科学家发现提高T细胞抗肿瘤免疫功能新方法
中科院上海生科院生物化学与细胞生物学研究所分子生物学国家重点实验室/国家蛋白质科学中心(上海)许琛琦研究组和分子生物学国家重点实验室李伯良研究组在一项合作研究中发现“代谢检查点”可以调控T细胞的抗肿瘤活性,并鉴定了肿瘤免疫治疗的新靶点——胆固醇酯化酶ACAT1以及相应的小分子药物前体,为开发新的肿瘤免疫治疗方法奠定了基础。今天,题为“通过调节胆固醇代谢增强CD8+T细胞的抗肿瘤反应”的研究成果







#科学家发现#
15
#新方法#
27
#中国科学#
16
#免疫功能#
0
#中国科学家#
17
牛
49
的确不错
136