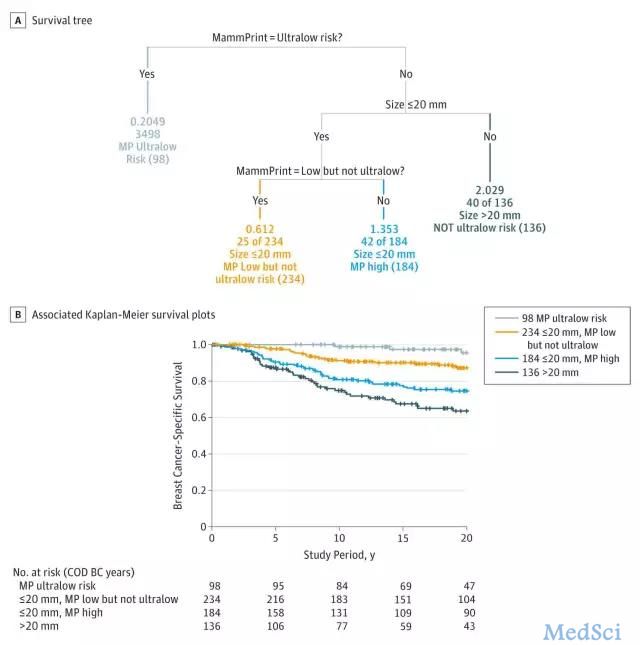
JAMA Oncology:何种情况的乳腺癌患者应在X光筛查基础上联合乳腺超声或MRI?
2017-07-14 刘婧(放瘤娃) 肿瘤资讯
2017年乳腺癌筛查指南更新。虽然在新指南中,乳腺超声和核磁共振(MRI)仍然属于从属地位,但两者也在临床上广泛使用,那么什么样的人应该在乳腺X光筛查的基础上,使用这两种手段进行筛查呢?

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
34
#Oncology#
32
#乳腺癌患者#
21
学习了受益匪浅
58
学习了分享了
57