J Hypertens:肾动脉狭窄和左心室肥厚有啥关系?
2017-08-13 xing.T MedSci原创
该荟萃分析表明与高血压患者相比,RAS患者左心室肥厚的可能性增加,肾动脉血运重建对左心室结构具有有益的效应,是通过左心室重量指数显著降低来反映。
肾动脉狭窄(RAS)患者左心室肥厚(LVH)以及肾血管重建术后LVH消退的数据资料很少。近日,高血压领域权威杂志Journal of Hypertension上发表了一篇荟萃分析文章,研究人员进行了一项荟萃分析以提供关于这个临床相关问题的全面信息。
研究人员纳入了所有RAS患者通过超声心动图对LVH进行评估并与原发性高血压患者进行比较的文献,研究人员对肾动脉血管重建后左室(LV)质量指数的变化进行了评估。
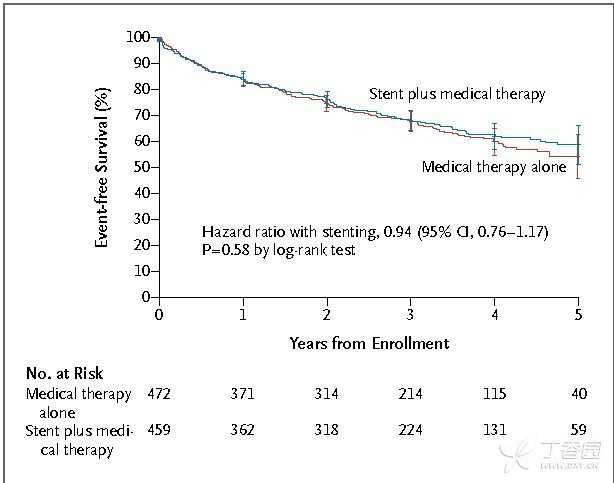
该荟萃分析共纳入了905名研究参与者(RAS为446人,原发性高血压患者为459人),共纳入了九项研究。RAS患者合并的左室质量指数明显高于原发性高血压患者(140.4±11.1克/平方米和121.8±6.2克/平方米,标准差为0.41±0.07 [95%可信区间(CI)为0.27-0.51,P<0.001]。在来自于八个研究中的360名接受了肾动脉重建的RAS患者中,基线和干预后合并的平均左室质量指数值分别为129±10.2克/平方米和115.5±9.9克/平方米,标准平均差为-0.36±-0.06(95%CI为-0.47至-0.25,P<0.001)。这些发现不受发表偏倚或单一研究效应的影响。
由此可见,该荟萃分析表明与高血压患者相比,RAS患者左心室肥厚的可能性增加,肾动脉血运重建对左心室结构具有有益的效应,是通过左心室重量指数显著降低来反映。
原始出处:
Cuspidi, Cesare,et al. Renal artery stenosis and left ventricular hypertrophy: an updated review and meta-analysis of echocardiographic studies.Journal of Hypertension. 2017. http://journals.lww.com/jhypertension/Abstract/publishahead/Renal_artery_stenosis_and_left_ventricular.97654.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#TENS#
26
#左心室肥厚#
36
#PE#
33
#心室肥厚#
32
#肾动脉#
46
#肾动脉狭窄#
34
继续学习中谢谢
63
谢谢分享.学习了很好!
55
认真学习,不断进步,把经验分享给同好。点赞了!
58
#左心室#
35