NEJM:肾动脉支架术不能预防不良肾脏和心血管事件
2014-03-03 清热解毒2号 丁香园
高血压人群肾动脉狭窄的发生率达到1%-5%,且通常合并有外周动脉疾病和冠心病,而基于社区筛查的研究结果发现肾动脉狭窄在65岁以上人群的患病率达7%。肾动脉狭窄有可能导致高血压、缺血性肾脏病及多种慢性并发症。 90年代的非对照试验表明,肾动脉成形术和支架术可显著降低收缩压和延缓慢性肾脏病进展。在1996年至2000年间,美国医保受益人群接受肾动脉支架术的手术量每年增长达364%。然而,三项
高血压人群肾动脉狭窄的发生率达到1%-5%,且通常合并有外周动脉疾病和冠心病,而基于社区筛查的研究结果发现肾动脉狭窄在65岁以上人群的患病率达7%。肾动脉狭窄有可能导致高血压、缺血性肾脏病及多种慢性并发症。
90年代的非对照试验表明,肾动脉成形术和支架术可显著降低收缩压和延缓慢性肾脏病进展。在1996年至2000年间,美国医保受益人群接受肾动脉支架术的手术量每年增长达364%。然而,三项关于肾动脉成形术的随机试验并未显示出血压获益,随后的两项肾动脉支架术的随机试验也并未达到肾功能改善。至今尚未有研究评估关于此项手术的临床结局,肾动脉支架术能否预防主要不良肾脏和心血管事件仍不确定。
为此,美国托莱多大学的Christopher J. Cooper等进行了一项随机对照试验,以评估肾动脉支架术及药物治疗对动脉粥样硬化性肾动脉狭窄患者临床事件的影响,相关研究发表于《新英格兰医学杂志》。
研究者纳入了947名合并有收缩期高血压或慢性肾脏病的动脉粥样硬化性肾动脉狭窄的患者(收缩期高血压患者服用2种或2中以上的降压药)。研究人员将患者随机分配至单纯药物治疗组和肾动脉支架术治疗合并药物治疗组。然后随访观察患者的不良心血管事件和肾脏事件。
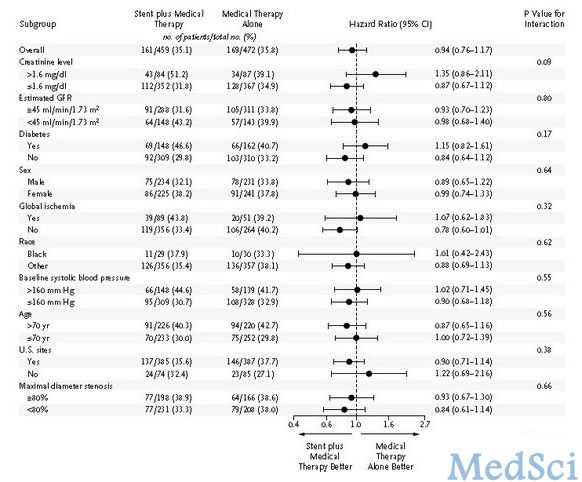
亚组间治疗效果的森林图
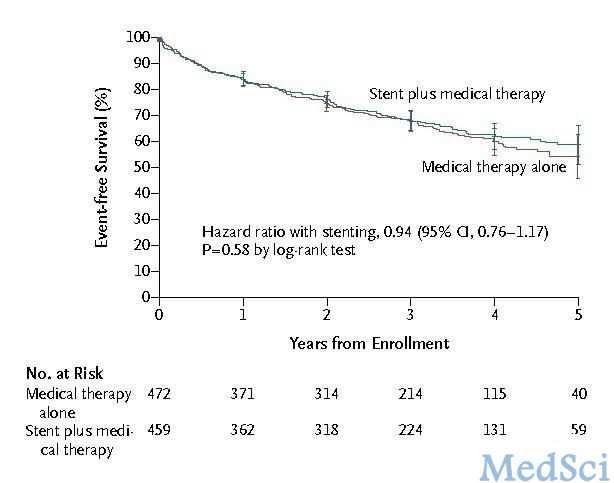
经过中位43个月的随访后,两组间的主要复合终点事件发生率无明显差异。同样,两组间的单个主要终点事件和全因死亡率也无明显差异。随访期间,肾动脉支架术治疗合用药物治疗组的收缩压均有轻微下降。
该研究认为,肾动脉支架合用多种全面的药物治疗不能预防合并收缩期高血压、或慢性肾脏病的动脉粥样硬化性肾动脉狭窄患者的临床事件。
原始出处:
Cooper CJ1, Murphy TP, Cutlip DE, Jamerson K, Henrich W, Reid DM, Cohen DJ, Matsumoto AH, Steffes M, Jaff MR, Prince MR, Lewis EF, Tuttle KR, Shapiro JI, Rundback JH, Massaro JM, D'Agostino RB Sr, Dworkin LD; CORAL Investigators.Stenting and medical therapy for atherosclerotic renal-artery stenosis.N Engl J Med. 2014 Jan 2;370(1):13-22. doi: 10.1056/NEJMoa1310753. Epub 2013 Nov 18.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肾动脉#
52
#支架术#
45
#肾动脉支架#
46
#血管事件#
54