中国NMPA:批准Pellino-1抑制剂BBT-401治疗溃疡性结肠炎的IND
2019-12-28 Allan MedSci原创
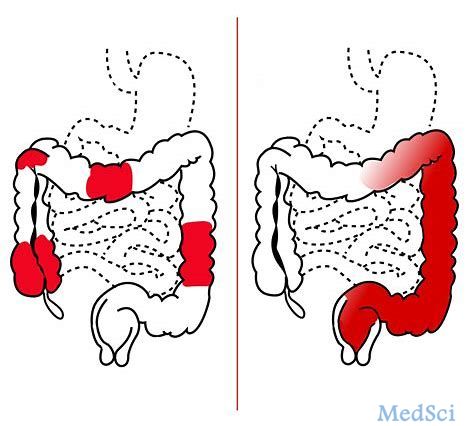
韩国制药公司Bridge近日宣布,中国国家药品监督管理局(NMPA)药品评审中心(CDE)批准了于2019年9月25日提交的IND,旨在寻求Pellino-1抑制剂BBT-401治疗溃疡性结肠炎(UC)的临床研究。
韩国制药公司Bridge近日宣布,中国国家药品监督管理局(NMPA)药品评审中心(CDE)批准了于2019年9月25日提交的IND,旨在寻求Pellino-1抑制剂BBT-401治疗溃疡性结肠炎(UC)的临床研究。Bridge计划于2020年5月开始在中国受试者中进行BBT-401的I期研究。该研究将以单次或多次递增口服剂量评估候选药物的安全性、耐受性和药代动力学特征。
根据2018年12月签署的许可和共同开发协议,该公司与日本大雄制药达成合作伙伴关系,共同开发BBT-401。大雄制药获得了包括中国在内的22个亚洲国家的BBT-401开发和商业化的独家权利。
原始出处:
https://www.firstwordpharma.com/node/1690169
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#溃疡性#
32
#抑制剂#
29
#PE#
38
#治疗溃疡性结肠炎#
35
#IND#
29
#PEL#
0