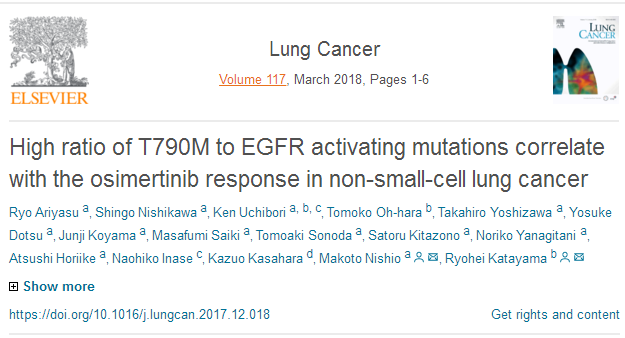
激荡20年:肺癌靶向治疗研究进展里程碑(下)
2018-02-20 肿瘤资讯编辑部 肿瘤资讯
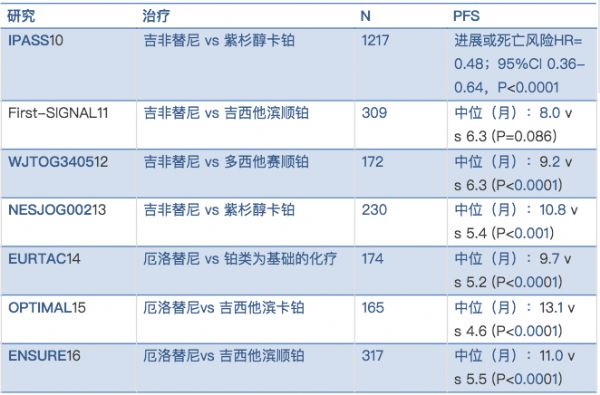
随着基因组学研究的进展,与肺癌相关的基因突变,从1984年发现KRAS突变后,不断涌现,基于驱动基因的靶向药物问世引领了肺癌治疗史上的重要变革。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






学习一下
81
学习了感谢分享
58
#里程碑#
28
#肺癌靶向治疗#
42
学习了.谢谢分享
0
#研究进展#
24
赞.有心了
68