EAU18∣叶定伟教授团队进一步明确了外科治疗在肾上腺皮质癌中的重要作用
2018-03-22 肖文军 肿瘤瞭望
肾上腺皮质癌是一种较为少见的疾病,但是恶性程度很高,预后较差,给患者及家属带来的疾病负担较大。美国SEER数据库的病例数较多,随访数据较为完善,随访时间也较长。因此,叶定伟教授团队利用这一数据库对肾上腺皮质癌的预后进行分析。该研究入选EAU18壁报展示(Poster NO.25)。
肾上腺皮质癌是一种较为少见的疾病,但是恶性程度很高,预后较差,给患者及家属带来的疾病负担较大。美国SEER数据库的病例数较多,随访数据较为完善,随访时间也较长。因此,叶定伟教授团队利用这一数据库对肾上腺皮质癌的预后进行分析。该研究入选EAU18壁报展示(Poster NO.25)。
叶定伟教授团队在SEER数据库中筛选2010到2014年间确诊为肾上腺皮质癌的18岁以上患者。收集临床及病理资料包括:性别、诊断时的年龄、种族、婚姻状况、诊断时间、手术与否、临床分期、肿瘤大小与生存状况等。进行生存分析并计算条件生存概率。
结果共有353例患者符合条件,其中112例诊断时已发生远处转移。诊断时发生远处转移的患者中位生存期为6月,未发生远处转移者为40月。Cox比例风险回归分析表明,高龄、高肿瘤分级、诊断时即有远处转移、没有接受手术是预后差的独立因素。对于确诊时没有远处转移的患者,年龄、肿瘤分级、淋巴结转移与否、是否接受手术是独立预后因素。对于确诊时有远处转移的患者,年龄、是否接受手术是独立预后因素
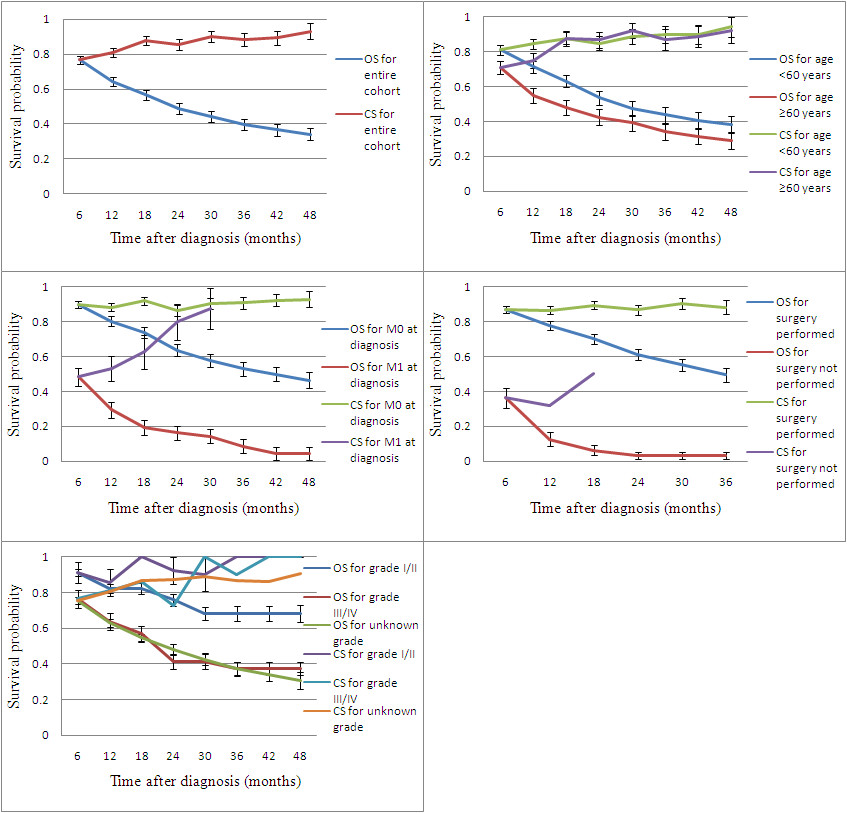
疾病的预后是随时间变化的,可以采用条件生存概率(conditional survival probability, CS)来对这一现象进行描述。CS被定义为患者已经存活了一定时间(X)的条件下,再存活另外一段时间(Y)的概率,可以表示为CS(Y / X)。如果患者已经存活X年,对应的概率为S(X)。S(X + Y)表示存活X + Y年的概率。那么在第X年时,该患者再存货Y年的概率CS(Y / x)= S(x + Y)/S(x)。
在本研究中,在诊断后的最初5年,存活18个月后的患者再存活半年的概率增加到约90%,而传统方法计算的总生存概率逐渐从大约80%下降到40%。另外随着时间的推移,大部分的不同预后因素组再存活半年的条件概率逐渐趋近,差异甚至消失。预后较差的患者亚组(如年龄较大,诊断即有远处转移) 条件生存概率的改变更为明显。不过对于没有接受手术治疗的患者,很少存活过18个月,条件生存概率始终未能改善。这充分说明是否接受手术是重要的预后因素,也显示了外科治疗在肾上腺皮质癌中的关键作用。
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肾上腺皮质癌#
33
#叶定伟#
44
#肾上腺#
34
#EAU#
44
#重要作用#
25
这个应该是没有疑义
60