一、二尖瓣瓣膜病
(一)二尖瓣狭窄(Mitral stenosis,简称MS)(图4-6)
风湿性心脏病引起二尖瓣受累可达100%(国内尸检资料)。单纯二尖瓣狭窄时,左房内血液不易流入左室,左房压力升高可逆传肺静脉,引起肺淤血,为克服其阻力,肺动脉压也相应升高,从而增加右心的负荷,引起肺动脉扩张及右心室增大。

图4-6 二尖瓣狭窄
后前位:心脏呈“二尖瓣”型。左心缘出现四个弧度,主动脉结小,肺动脉段隆凸,左心耳呈舌样突出,左室不大而右室增大,心尖位于膈上。右心缘有“双心房”征。两肺有肺淤血征。
右前斜位:食管的左房压迹加深并后移,心后间隙变窄。肺动脉圆锥及右心室向前隆凸。
左前斜位:早期无异常。重度左房增大可将左主管气管向上抬高。右室增大使心前缘下段向前隆凸。
(二)二尖瓣狭窄及关闭不全(Mitral stenosis and incompetence,简称MS+MI)
单纯二尖瓣关闭不全少见,常与狭窄并存。当左心室收缩时,由于二尖瓣关闭不全,致使部分血液逆流入左房,左房排血发生障碍,负荷加重,因而左房扩大比单纯二尖瓣狭窄更为明显。肺血管早期表现脉淤血,继之可出现肺动脉高压。
X线征(图4-7):
以二尖瓣狭窄为主。关闭不全较轻者,其X线表现和单纯二尖瓣狭窄相似,并有轻度左室增大;以二尖瓣关闭不全为主,X线表现左房高度增大,左心室向左下延伸,右室亦增大。左前斜位见心后缘下段向后下增大与脊椎重叠较多。心前下缘向前变园隆。两肺表现肺淤血及肺动脉高压征。

图4-7 二尖瓣狭窄及关闭不全
二、主动脉瓣瓣膜病
(一)主动脉瓣狭窄(Aortic stenosis,AS)
多因风湿病引起,亦可见先天性主动脉瓣发育障碍,瓣口窄小,可伴有瓣下(即左心室流出道)狭窄。
X线征:心脏呈“主动脉瓣”型,主动脉结正常,心腰凹陷。心脏轻~中度增大。因左室增大以肥厚为主,致左室上部较凸出,心尖圆钝,左室搏动增强。升主动脉中下段敢局限性扩张90%以上病例有搏动增强。左室造影能显示瓣膜形态及瓣口大小,亦能显示左室流出道有无狭窄等,为确诊本病的主要检查的方法。
(二)主动脉瓣关闭不全(Aortic insufficiency,AI)
多因风湿病引起,先天性发育异常少见,可因主动脉窦脱垂导致瓣膜关闭不全。
心脏舒张期,左心室不仅接受左心房的血液,而且接受从主动脉回流的血液,故左心室心腔扩张,同时伴有心肌肥厚。左心室容纳较多的血量,当心脏瞬间收缩时,主动脉接受较多的血液,因此,主动脉明显增宽,初期血管弹性完好,增宽是动力性的,舒张期仍能恢复,而且由于瓣膜漏血,主动脉管腔相对空虚。后期主动脉管壁损害,弹性消失,主动脉增宽是器质性的,舒张期回缩力减弱。
X线征(图4-8)

图4-8 主动脉瓣关闭不全
后前位:心脏呈“主动脉瓣”型,左室增大以扩张为主,左室向左下变园隆,心尖下移,心腰凹陷。主动脉扩张,透视下左室及主动脉搏动增强。
右前斜位:心前下缘隆凸,使心前间隙变窄或消失。
左前斜位:左心室增大表现心后缘下段向后隆凸,与脊椎重叠较多,室间沟前移。主动脉弓增宽,尢以升主动脉增宽明显。
三、联合瓣膜疾病(Combined vavular diseases)
风湿病多侵犯二尖瓣,同时也可侵犯主动脉瓣及三尖瓣,后者少见。
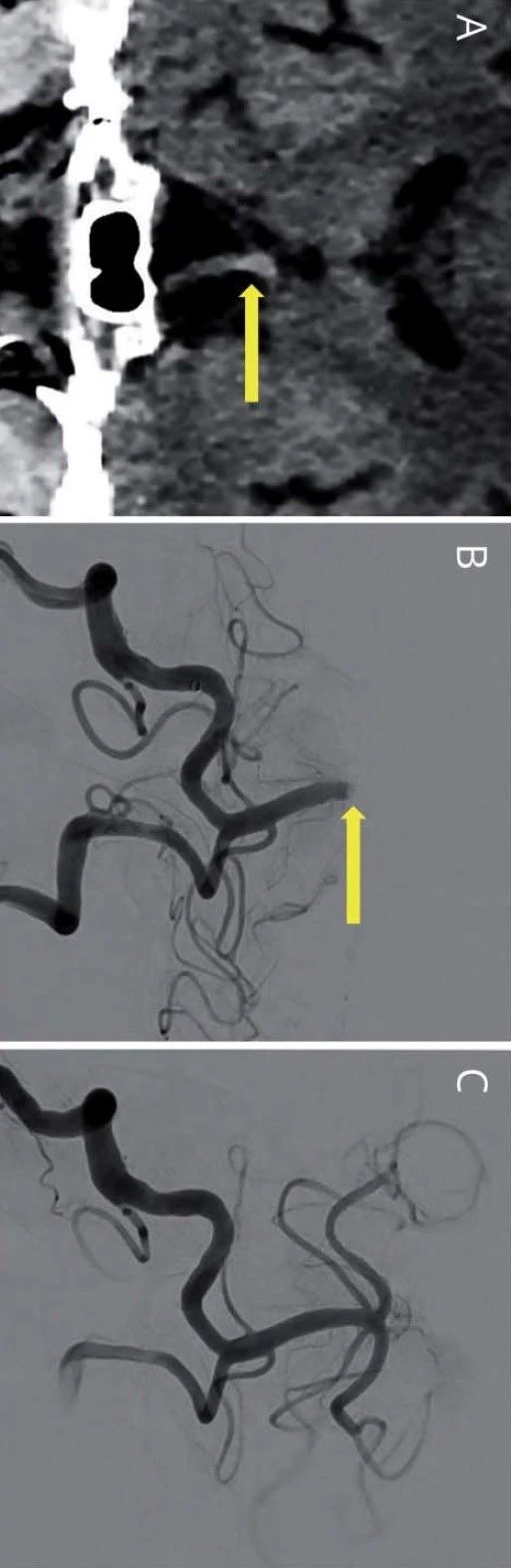
二尖瓣主动脉瓣联合瓣膜病(Combined mitral and aortic valvular diseases)
常见二尖瓣双损害与主动脉瓣闭锁不全合并存在,简称MS+MI+AI。
X线征(图4-9):心脏增大及肺淤血X线表现,兼有上述二尖瓣及主动脉瓣膜病的征象。如以二尖瓣狭窄为主,则显示肺动脉段隆凸及双心房征,斜位片显示食管受压,移位。肺淤血明显或具有肺循环高压。如以主动脉瓣关闭不全为主,则以左心室增大为主,主动脉搏动增强,左房轻度增大,肺动脉段平直或轻凸,肺淤血较轻。

图4-9 二尖瓣主动脉瓣联合瓣膜病
A.二尖瓣损害为主 B.主动脉瓣损害为主
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#心脏瓣膜#
35
#X线#
0
#心脏瓣膜病#
56
#瓣膜#
41