Obstet Gynecol:I期上皮性卵巢癌患者接受保留生育功能手术后的全因死亡率分析!
2017-06-23 xing.T MedSci原创
由此可见,在I期上皮性卵巢癌年轻女性中,与常规手术相比,保留生育功能手术并不会增加死亡风险。
近日,妇产科权威杂志Obstetrics and Gynecology上发表了一篇研究文章,研究人员旨在比较I期卵巢癌患者接受保留生育功能手术与接受常规手术的全因死亡率。
在使用国家癌症数据库的队列研究中,研究员选取了在2004年至2012年间诊断为IA期和单侧IC期上皮性卵巢癌的年龄小于40岁的女性作为研究对象。保留生育功能手术即为保留一侧卵巢和子宫。该研究的主要结局为从诊断到死亡的时间。研究人员使用倾向评分方法来构建一个接受保留生育功能或常规手术的妇女队列,但是在观察到的协变量上是相似的,并使用Kaplan-Meier方法和Cox比例风险模型进行生存分析。
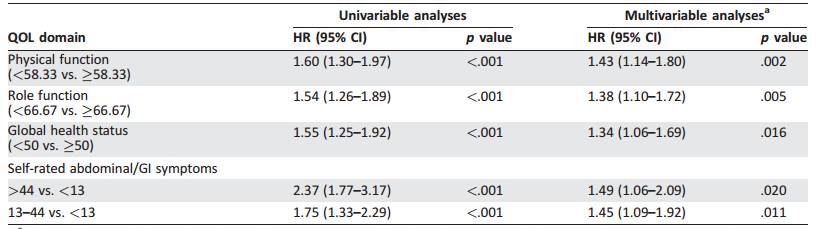
研究人员选择了1726名患IA期和单侧IC期上皮性卵巢癌的妇女,其中825例(47.8%)接受了保留生育功能手术。保留生育功能手术与较小的年龄、居住在美国东北部和西部、浆液性或粘液性组织学结果相关(P<0.05)。研究人员通过倾向评分匹配获得了一个有904名在观察协变量上保持平衡的女性队列。在中位随访63个月之后,接受保留生育功能手术的妇女中有30人死亡,接受常规手术的倾向匹配的妇女中有37人死亡。保留生育功能手术与死亡风险无相关性(风险比为0.80,95%可信区间为0.49-1.29,P =0 .36)。保留生育功能组诊断后10年生存率为88.5%(95%可信区间为82.4-92.6),常规手术组为88.9%(95%可信区间为84.9-92.0)。在具有高危特征:如透明细胞组织学、3级或IC期的患者中,接受保留生育功能手术的女性中10年生存率为80.5%(95%可信区间为68.5-88.3),而常规手术为83.4%(95%可信区间为76.0-88.7)(风险比0.86,95%可信区间为0.49-1.53,P=0.61)。
由此可见,在I期上皮性卵巢癌年轻女性中,与常规手术相比,保留生育功能手术并不会增加死亡风险。
原始出处:
Melamed, Alexander, et al. All-Cause Mortality After Fertility-Sparing Surgery for Stage I Epithelial Ovarian Cancer.Obstetrics & Gynecology.2017. http://journals.lww.com/greenjournal/Abstract/publishahead/All_Cause_Mortality_After_Fertility_Sparing.98387.aspx
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TET#
33
#NEC#
33
#皮性卵巢癌#
24
#上皮性卵巢癌#
38
学习了,谢谢分享
47
#全因死亡率#
23
学习了受益匪浅。
48
卵巢癌患者接受保留生育功能手术情况介绍
46