压力对于肿瘤进化是不可或缺的,癌细胞的生存依赖于压力的调节。
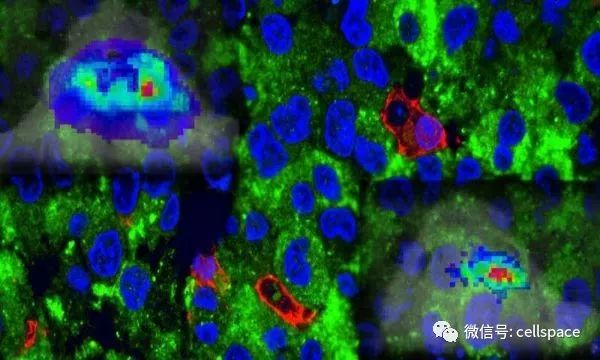
图片来源:Cincinnati Children's
而近日来自辛辛那提儿童医院医疗中心的研究人员领衔的一项研究就发现肿瘤相关的压力可以缓慢激活生物能量感受器AMP激酶(AMPK)。为了生存,癌细胞会劫持正常细胞中保守的一个调节AMPK的压力响应信号通路为肿瘤供能,相关研究于近日发表在《Nature Cell Biology》上,题为“AMP kinase promotes glioblastoma bioenergetics and tumour growth”。
通过对癌症基因组图谱项目中的数据进行分析,研究人员发现这种AMPK亚型在致命的人类癌症-恶性胶质瘤(GBM)中高表达。研究人员还发现抑制APMPK可以延缓病人来源GBM干细胞(GSCs)以及肿瘤的生长和活力。
在受压力(运动)的骨骼肌中,AMPK与cAMP反应元件结合蛋白1(cAMP response element binding protein-1,CREB1)一起激活,以促进葡萄糖代谢。研究人员发现致癌的压力会缓慢激活GSCs中的AMPK,并劫持AMPK-CREB1通路协调肿瘤的生物供能,主要通过转录因子HIF1和GABPA来完成。
最后研究人员发现成年小鼠可以耐受全身性清除AMPK,这表明使用AMPK抑制剂药物治疗GBM或许是一种新的选择。
原始出处:
Chhipa RR, Fan Q, Anderson J, et al.AMP kinase promotes glioblastoma bioenergetics and tumour growth.Nat Cell Biol. 2018 Jun 18. doi: 10.1038/s41556-018-0126-z. [Epub ahead of print]
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Bio#
35
#Biol#
35
#Nat#
37
#Cell#
29
#CEL#
24
#脑癌#
28
#抑制因子#
38
学习学习谢谢
46
研究人员发现成年小鼠可以耐受全身性清除AMPK.这表明使用AMPK抑制剂药物治疗GBM或许是一种新的选择
60
AMPK亚型在致命的人类癌症-恶性胶质瘤(GBM)中高表达
53