气候还能影响酒精性肝硬化?
2017-04-24 sunshine2015 来宝网
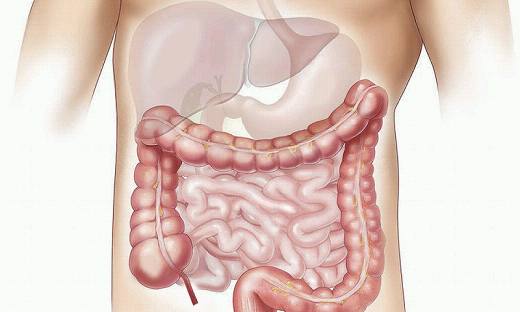
荷兰阿姆斯特丹2017年国际肝脏大会今天发布的新数据表明,世界上较冷和缺少阳光的地区,酒精性肝硬化发生率较高,酒精性肝硬化是由过度饮酒导致的肝脏不可逆转的瘢痕形成引起的疾病。一个来自190多个国家的国际科学家分析数据发现,每升高一摄氏度的温度与肝硬化的酒精归因分数(AAF *)下降0.3%有关。重度酒精摄入导致温暖的感觉,而较少的阳光接触与抑郁症有关,
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#酒精性#
39
#酒精性肝硬化#
55
学习了,谢谢分享
65
好好学习,涨知识
52
学习了很有用
67
很好,涨知识
62