恕我直言:这种癌症发生时,你竟还以为是犯痔疮!
2016-12-01 周小编 天津医科大学肿瘤医院
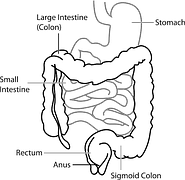
本期话题:如何辨识结直肠癌?都说十人九痔,但是,那些自以为犯痔疮的人想不到,或许,这正是一种癌症的早期信号!大众都会以为,痔疮会有便血,但是在肠道肿瘤发生时也会有!如果能及时区分辨认便血的缘由就能尽早发现这种恶性肠道肿瘤!然而,又有多少人一听说做肠镜检查,就蔫儿了呢……恕我直言,结直肠癌的早期症状也有便血。一旦发现便血症状,应尽早到医院检查,确认造成便血的病因,究竟是痔疮,还是结直肠癌要点一便血意
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#痔疮#
39
这个标题,,,相当动人啊
73
讲的挺好!
83
简单明了,一看就懂
64
很有意思的文章,涨知识,也打开我的误区!非常精彩!
83