ERJ:心肺运动试验在肺静脉闭塞性疾病诊断中的作用
2021-10-10 刘少飞 MedSci原创
肺静脉闭塞性疾病 (PVOD) 是一种罕见的肺动脉高压,与特发性肺动脉高压 (PAH) 具有一些临床和血液动力学特征。然而,考虑到 PAH 特异性治疗可能会导致危及生命的肺水肿,因此怀疑 PVOD 至

肺静脉闭塞性疾病 (PVOD) 是一种罕见的肺动脉高压,与特发性肺动脉高压 (PAH) 具有一些临床和血液动力学特征。然而,考虑到 PAH 特异性治疗可能会导致危及生命的肺水肿,因此怀疑 PVOD 至关重要,因此诊断时应考虑肺移植。
EIF2AK4 基因中不存在致病性变异,并且在这些患者中进行肺活检的风险很高,这通常会妨碍 PVOD 的明确诊断。因此,PVOD 诊断通常依赖于与 PVOD 相关可能性高的其他指标的识别,即:肺一氧化碳扩散能力 (DLCO) 和典型的高分辨率计算机断层扫描 (HRCT) 特征。然而,它们的敏感性和特异性远非完美,并且缺少额外的诊断工具。该研究假设心肺运动测试 (CPET) 可能揭示 PVOD 患者运动表现的特征模式,加强其怀疑和诊断。
针对23 名被诊断为 PVOD 的患者,这些患者被转诊至国家肺动脉高压转诊中心。其中,16名患者携带EIF2AK4致病性双等位基因变异;2个出现了典型的 HRCT 三个特征;2人在 PAH 特异性治疗中出现肺水肿;并且,在其余3个中,PVOD 诊断只能通过移植后肺标本的组织学检查来进行。对照组由 52 名接受定期随访的连续 PAH 患者组成(24 名特发性 PAH 和 28 名与 BMPR2 相关的遗传性 PAH)。
患者在自行车测力计上接受了症状限制的增量 CPET。在休息时测量运动变量、通气阈值和运动峰值。通过脉搏血氧仪监测氧饱和度。分析了最接近 CPET 的临床和血液动力学数据。平均年龄为39.8±11.9 年,PVOD组和PAH组之间没有差异。 PVOD 患者没有表现出女性优势。他们表现出较差的功能等级 (FC)和较低的 DLCO 水平比 PAH 患者。大多数 CPET (85.3%) 是在接受 PAH 特异性治疗的患者中进行的,其中 32% 的患者接受全身前列环素治疗。 11 名患者未接受任何 PAH 特异性药物治疗:9 名(7 名 PAH 和 2 名 PVOD)在诊断时接受了 CPET,2 名 PVOD 不能耐受。与 PAH 相比,PVOD 患者在通气阈值时的预测峰值摄氧量 (VO2)、氧脉冲和 VO2 水平显着降低。

尽管与 PVOD 相关的运动能力和预后较差,但各种研究并未观察到 PVOD 和 PAH 之间的血流动力学差异。此外,我们的研究实际上表明 POVD 人群的肺压显着降低。重要的是,之前的研究观察到 CPET 参数与 PAH 的血流动力学严重程度之间存在关联。然而,在我们的研究中,VO2 的降低和通气效率低下的程度似乎都与 PVOD 患者的血流动力学严重程度不成比例,支持了 PVR 之外的其他因素在其病理生理学中起关键作用的假设。
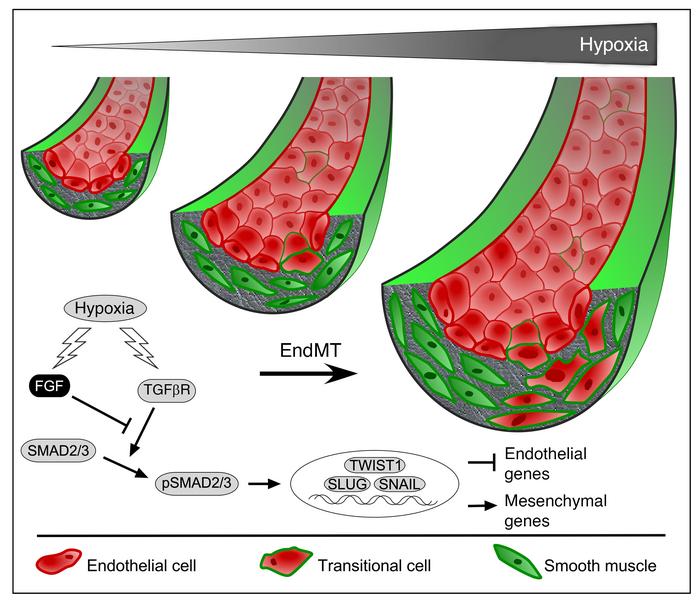
PVOD一些可能的机制。
1) PVOD中发生的血管重构,包括小静脉内膜纤维化、小静脉肌肉增生和毛细血管增生,导致肺毛细血管血容量和肺泡膜扩散降低。这些改变与血液动力学严重程度无关,并反映在 DLCO 值降低。
2) 毛细血管充血和间质水肿减少气体交换,进一步损害通气效率
3) 运动过程中显着的低氧血症会加剧心肌缺血和右心室衰竭,并可能证明 PVOD 中氧脉冲的扁平行为是合理的,尽管静息时心输出量正常
4) 低氧血症和低心输出量减少外周氧输送并诱发乳酸酸中毒的早期发作,导致早期通气阈值和较低的 VO2 。
总之,PVOD 和 PAH 显示出不同的运动模式,其中血液动力学与功能和通气障碍之间的不成比例变化尤其令人感兴趣。 预测的 VO2、VE/VCO2 斜率和 PVR 的组合显示出准确识别 PVOD 的最高能力,将 CPET 定位为有前途的 PVOD 无创诊断的附加工具。
文章出处:
Pérez-Olivares C. The role of cardiopulmonary exercise test in identifying pulmonary veno-occlusive disease. Eur Respir J. 2021 Jun 4;57(6):2100115. doi: 10.1183/13993003.00115-2021. PMID: 33653804.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#疾病诊断#
50
#心肺#
63
#心肺运动试验#
47
#运动试验#
40
#静脉#
39