JCI:骨折愈合机理研究,推翻传统理论!
2015-08-18 佚名 生物探索
医学上一直认为血纤维蛋白(Fibrin)作为一种凝血因子,在骨折愈合中发挥重要作用。但是,8月3日发布于the Journal of Clinical Investigation的最新学术论文却推翻了这一论断,证实在骨折恢复过程中,血纤维蛋白并不必要,相反该蛋白的降解才真正有利于骨头再生。骨组织是身体分布血管最多的部位。当骨头发生碰撞骨折,会严重挤压、破坏血管。而血纤维蛋白会促进血液凝固,防止骨折
医学上一直认为血纤维蛋白(Fibrin)作为一种凝血因子,在骨折愈合中发挥重要作用。但是,8月3日发布于the Journal of Clinical Investigation的最新学术论文却推翻了这一论断,证实在骨折恢复过程中,血纤维蛋白并不必要,相反该蛋白的降解才真正有利于骨头再生。
骨组织是身体分布血管最多的部位。当骨头发生碰撞骨折,会严重挤压、破坏血管。而血纤维蛋白会促进血液凝固,防止骨折造成的血管破裂血流不止。所以,过去的研究一直坚信血纤维蛋白促进骨肉痊愈,为其愈合提供一个骨头再生的初始支架。
但是范德堡大学医学中心研究团队最新发现:即便缺少血纤维蛋白前体——纤维蛋白原,小鼠依旧能够正常进行骨折修复过程。这与教科书上的内容大大相悖!
血纤维蛋白不利于骨折愈合
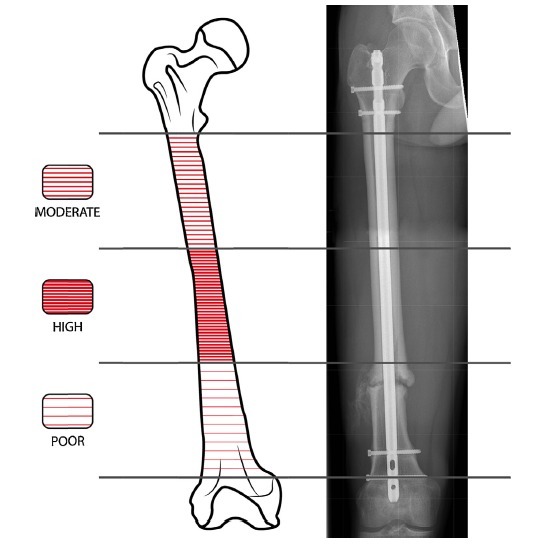
该研究团队之前就发表过血管再生对于骨折恢复很重要的学术论文。通过成像技术,他们对新血管生成和骨折后骨头修复进行同时观察发现,骨头血管会在骨折末端位置先于新骨头生成、延伸联接。
而且,研究人员还发现,试验小鼠如果不能降解血纤维蛋白,会出现异位骨化,从而阻碍创伤或者骨科手术后的恢复过程。由此推测,如果血纤维蛋白不能有效降解,会阻滞骨折愈合。研究人员表示,对于研究成果完全意外,血纤维蛋白的降解对于防止异位骨化至关重要。
现实却是:骨折会阻滞血纤维蛋白降解!这也就是为什么骨伤痊愈缓慢的原因之一。这个研究发现可以解释为什么孩子骨折恢复较快——因为他们的纤维蛋白原水平只有成年人的一半。这一发现也许还能够解释为什么肥胖者、糖尿病患、吸烟的人、老年人骨折愈合缓慢。
应用前景
依据这项出乎意料的研究结果,研究团队设想:如果能够降低纤维蛋白原的含量,或者增加纤维蛋白降解酶的活力,那么成年人将会拥有等同于孩子的愈合能力。所以,为了将原理付诸于实践,该团队正在努力研发骨生物活性材料,用于增强降解血纤维蛋白。
范德堡大学骨科手术和康复学教授、医学博士Jonathan Schoenecker说:“目前,很多药物的研发建立在通过血纤维蛋白促进骨折愈合的原理上。在某些情况下,它可能会有所帮助。但是我们肯定的是你并不需要它,骨折修复并不需要血纤维蛋白。相反,某种意义上讲,研制防止血凝的药物可能会促进组织修复和再生。”
文章来源:
Masato Yuasa.et al.Fibrinolysis is essential for fracture repair and prevention of heterotopic ossification.JCI.2015
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











看来活血化瘀,不是没有意义的
50
#骨折愈合#
35
真的这么简单?
118
长见识
115
#JCI#
26
希望该理论运用到临床
163
不错,赞一个
76
新颖
71
学习了…
131
实用实用!
89