Cancer Cell:杀灭癌细胞的新药物NSC319726被发现
2012-05-19 T.Shen 生物谷
近日,刊登在国际著名杂志Cancer Cell上的一项研究表明,一种化合物可以通过修复人类癌症突变蛋白(肿瘤抑制基因p53编码)的结构和功能来有选择性的杀灭癌细胞。文章中,研究者识别出了一种新的潜在的抗癌药物,这种药物以常见的第三个突变的p53基因-p53-R175H为靶点。 在人类机体中,p53可以识别细胞压力以及及时控制细胞增值,或者杀灭不能进行自我损伤修复的细胞。在近乎一半的癌症病人身上,

近日,刊登在国际著名杂志Cancer Cell上的一项研究表明,一种化合物可以通过修复人类癌症突变蛋白(肿瘤抑制基因p53编码)的结构和功能来有选择性的杀灭癌细胞。文章中,研究者识别出了一种新的潜在的抗癌药物,这种药物以常见的第三个突变的p53基因-p53-R175H为靶点。
在人类机体中,p53可以识别细胞压力以及及时控制细胞增值,或者杀灭不能进行自我损伤修复的细胞。在近乎一半的癌症病人身上,编码p53的基因都突变了,p53功能的缺失会引起一系列的癌症症状,比如癌细胞具有侵袭性、转移性、对化学疗法或者放射疗法低敏感性,用药物恢复p53的功能被认为是未来潜在的治疗癌症的方法,然而,很难找到一种化合物来恢复肿瘤抑制基因p53的功能。
Alexei Vazquez博士表示,他们基于电脑筛选的方法找到了一种化合物,可以以肿瘤细胞p53为靶点,但是并不以正常细胞的p53为靶点。研究者的这种筛选方法比较独特,因为这涉及了癌细胞的多种遗传背景,研究者识别出的化合物可以杀死含有p53基因突变的癌细胞,其中有一种化合物可以恢复基因p53-R175H的突变,而且研究者确保人体的正常细胞是不会受这种化合物影响的。
此外,识别出的这种化合物可以有选择性的恢复突变基因p53-R175H的功能,研究者的发现同样支持了靶向癌症治疗的方法,研究者Carpizo表示,我们的研究发现将为未来的癌症治疗提供重要的线索和建议,未来,病人癌症的治疗效率将依赖于病人癌症的基因型差别。

doi:10.1016/j.ccr.2012.03.042
PMC:
PMID:
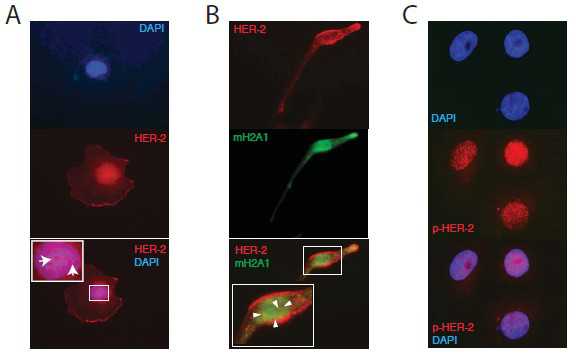
Allele-Specific p53 Mutant Reactivation
Xin Yu, Alexei Vazquez, Arnold J. Levine, Darren R. Carpizo
Rescuing the function of mutant p53 protein is an attractive cancer therapeutic strategy. Using the National Cancer Institute's anticancer drug screen data, we identified two compounds from the thiosemicarbazone family that manifest increased growth inhibitory activity in mutant p53 cells, particularly for the p53R175 mutant. Mechanistic studies reveal that NSC319726 restores WT structure and function to the p53R175 mutant. This compound kills p53R172H knockin mice with extensive apoptosis and inhibits xenograft tumor growth in a 175-allele-specific mutant p53-dependent manner. This activity depends upon the zinc ion chelating properties of the compound as well as redox changes. These data identify NSC319726 as a p53R175 mutant reactivator and as a lead compound for p53-targeted drug development.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#CEL#
32
#cancer cell#
32
#新药物#
29
#Cell#
26
#癌细胞#
27