JACC:CAR-T疗法与不良心血管事件的相关性研究
2019-12-21 不详 MedSci原创
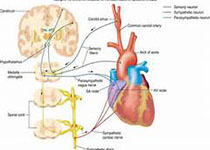
嵌合抗原受体重定向T细胞(CAR-T)用于靶向治疗肿瘤细胞,本研究的目的旨在评估CAR-T可能的心脏毒性。本研究纳入分析了137名接受了CAR-T治疗的患者,心脏毒性定义为左室射血分数的降低或血清肌钙蛋白水平的增高。患者的平均年龄为62岁(男性占67%,88%患有淋巴瘤,8%患有骨髓瘤)。近50%的患者接受的是商业CAR-T治疗,剩下的接受的是非商业CAR-T治疗。细胞因子释放综合征(CRS)出现
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#血管事件#
34
#CAR-#
30
#相关性#
25
#JACC#
40
#ACC#
24
好好好好好好
92