JAMA Surg:非前哨淋巴结阳性或为黑色素瘤不良预后的预测因子
2013-08-08 SHUMUFENG dxy
研究要点: 前哨淋巴结阳性的预测因素包括年龄、Breslow厚度以及溃疡情况。 前哨淋巴结阳性患者中位总生存期为178个月,非前哨淋巴结阳性患者则为42.2个月。 非前哨淋巴结阳性与复发、总生存期更短及黑色素瘤特异性生存期更短相关。 III期黑色素瘤患者的生存期差异很大。非前哨淋巴结(NSLN)状态具有临床意义,因而可考虑将其作为更好的生存预测因子合并入美国癌症联合委员
研究要点:
前哨淋巴结阳性的预测因素包括年龄、Breslow厚度以及溃疡情况。
前哨淋巴结阳性患者中位总生存期为178个月,非前哨淋巴结阳性患者则为42.2个月。
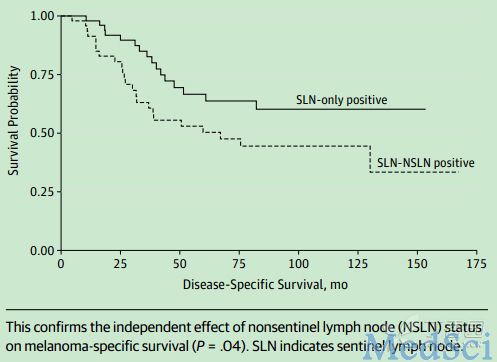
非前哨淋巴结阳性与复发、总生存期更短及黑色素瘤特异性生存期更短相关。
III期黑色素瘤患者的生存期差异很大。非前哨淋巴结(NSLN)状态具有临床意义,因而可考虑将其作为更好的生存预测因子合并入美国癌症联合委员会(AJCC)癌症分期系统。【原文下载】
加拿大圣莫尼卡圣约翰医学中心John Wayne癌症研究所的Mark B.Faries博士等人对此进行了深入研究,他们发现,非前哨淋巴结阳性是III期黑色素瘤患者最有临床意义的预后因子之一。黑色素瘤NSLN状态亚组分析应考虑纳入美国癌症联合委员会癌症分期系统。相关论文发表于国际权威杂志JAMA2013年7月29日在线版。
该研究旨在评估仅有前哨淋巴结(SLNs)扩散的黑色素瘤较扩散至非前哨淋巴结是否具有不同的临床意义。研究者入组患者展开问卷调查。主要结局指标包括无疾病生存期、黑色素瘤特异性生存期(MSS)及总生存期。
结果显示,从1986年到2012年,总共有4223例患者接受SLN活检。其中329例患者呈现SLN阳性。在上述329例患者中,有250例患者NSLN阴性,79例患者阳性。NSLN阳性的预测因素包括老龄、更高的Breslow厚度以及溃疡。单一SLN阳性组患者中位总生存期为178个月,NSLN阳性组则为60个月。多变量分析显示,NSLN阳性与复发风险、更短的总生存期及更短的MSS的关联更强。
研究得出如下结论,非前哨淋巴结阳性是III期黑色素瘤患者最有临床意义的预后因子之一。黑色素瘤NSLN状态应考虑纳入美国癌症联合委员会癌症分期系统。
研究背景:
SLN活检可以检出20%的隐匿性淋巴结转移,这一结果已得到既往研究的验证。现行指南的观点是所有阳性SLN患者均应行完全淋巴结清除术(CLND),原因是缺乏检出非前哨淋巴结转移的可靠工具,然而,CLND会增加血肿、感染、神经损伤和淋巴水肿的风险。且80%至90%CLND术后患者无额外阳性结节。考虑至这一低阳性率,不少研究者已开始质疑CLND是否必须。
尚未证实NSLNs是否代表着不同级别的淋巴结目前尚未明确。若干近期研究,提示阳性NSLN预示结局不良。综上,即使CLND不一定改善生存,它也可以为预后分期提供有价值的额外信息。
2009年美国癌症联合委员会(AJCC)更新了有关黑色素瘤分期的官方指南。III期黑色素瘤的现行AJCC分期标准考虑的指标包括:原发灶肿瘤溃疡和破裂,淋巴结肿瘤负荷等。上述标准未考虑阳性结节是否为前哨或非前哨。

【原文下载】Donovan CA, Pommier RF, Schillace R, O'Neill S, Muller P, Alabran JL, Hansen JE, Murphy JA, Naik AM, Vetto JT, Pommier SJ.Correlation of Breast Cancer Axillary Lymph Node Metastases With Stem Cell Mutations.
JAMA Surg. 2013 Jul 24. doi: 10.1001/jamasurg.2013.3028. [Epub ahead of print]PMID:
- 23884447
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#色素#
24
#淋巴结#
22
#预测因子#
30
#不良预后#
30
#淋巴结阳性#
34
#前哨淋巴结#
27
#黑色素#
23
#黑色素#
19