Int Forum Allergy Rhinol:非囊性纤维化性支气管扩张患者的慢性鼻窦炎的患病率和鉴定
2019-10-19 AlexYang MedSci原创
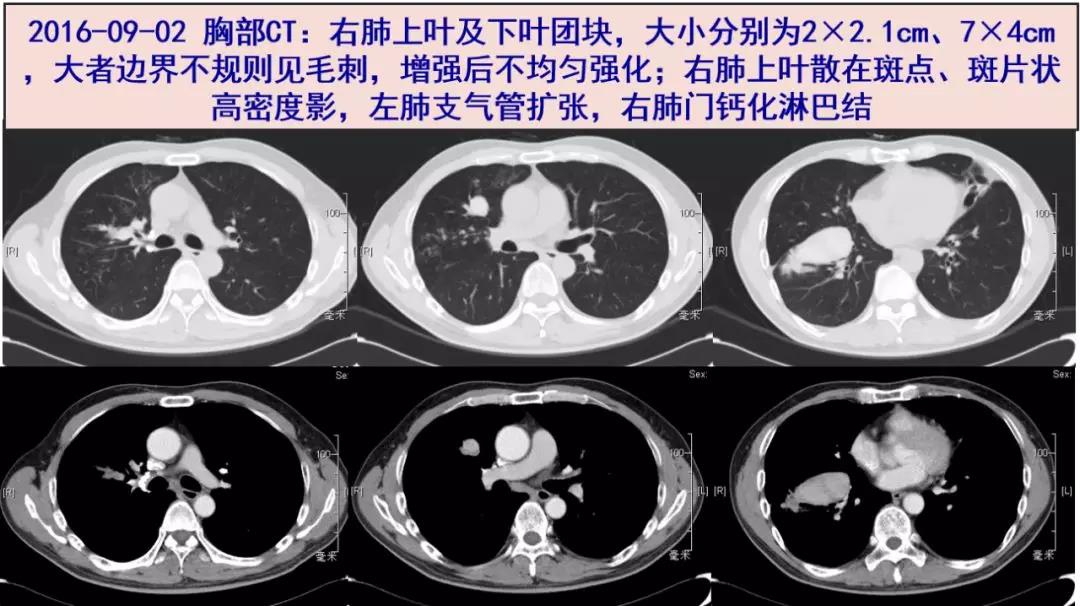
慢性鼻窦炎(CRS)与支气管扩张相关;然而,该相关性在美国(US)人群中仍没有很好的研究。最近,有研究人员确定了CRS在患有支气管扩张患者中的流行度情况,并鉴定了哪一种并发疾病与支气管扩张患者的CRS的存在相关。研究是一个回顾性的群体研究,数据从一个大的数据库中获得。研究人员鉴定了2007年到2017年患有支气管扩张的患者。研究人员根据伴随的CRS的有无将患者分成了2个群体。特征鉴定分析包括了人口
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#囊性#
29
#扩张#
35
#支气管#
42
#患病率#
42
#ALL#
0
#慢性鼻窦炎#
38